* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Slide 1
Psychopharmacology wikipedia , lookup
Specialty drugs in the United States wikipedia , lookup
Pharmaceutical marketing wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Drug design wikipedia , lookup
Medical prescription wikipedia , lookup
Pharmacognosy wikipedia , lookup
Compounding wikipedia , lookup
Drug discovery wikipedia , lookup
Neuropharmacology wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Theralizumab wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Prescription costs wikipedia , lookup
Drug interaction wikipedia , lookup
Adherence (medicine) wikipedia , lookup
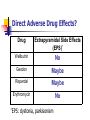
Perilous in Partnering Polypharmacy Medication Safety Kevin L. Wallace, MD, FACMT Assoc. Professor, Dept. of Pharmacy Practice UNE College of Pharmacy April 29, 2011 Presentation Objectives Increase awareness of polypharmacy-related risk factors and impact on patient outcome. Promote use of safe and cost-effective medication therapy management tools and strategies. Support interprofessional collaboration and active patient involvement in care management. Case 20 yo college student admitted for chief complaint of several week-duration morning stiffness, unsteady gait, and dysphoria. PMH: bipolar disorder; gastroesophageal reflux disorder (GERD) Medications: Geodon 60 mg BID Wellbutrin SR 150 mg QAM Risperdal 2 mg QHS E-mycin 333 mg TID Case (cont’d) Failed GERD treatment with Reglan due to “muscle stiffness” innate susceptibility to D2 antagonistinduced dystonia/movement disorder? Started on promotility GERD therapy (oral erythromycin) about 2 months prior to this admission. ADE determinant? Adverse Drug Events (ADE) ADE = medicationrelated injury Highly vulnerable groups include: Elderly (>65 yrs) Younger adults/adolescents with psychobehavioral disorders Infants/toddlers “Collateral Damage” ADE Incidence & Impact U.S. Population Approx. 500,000 Medicare patient ADEs/yr in outpatient setting 5th leading cause of death Estimated cost: ~ $300 billion/yr Patient quality of living cost of care Gurwitz et al 2003; NEHI 2009 Major Risk Factor: Drug Provision http://www.medscape.com/viewarticle/724186_print ADE Risk Determinants Drug-related Mechanism(s) of action and potency Dose Formulation Route of administration Frequency and duration of use Patient-related Age Genetic makeup Psychosocial factors Other underlying medical disorders Exposure to other substances (e.g., interacting nonpharmaceuticals) Number of drugs in treatment regimen = most potent ADE risk factor! Polypharmacy – Definition? >4 drugs per regimen May/may not include nonprescription (aka, “OTC”: over-the-counter) medications and other supplements Common OTC ADEs acetaminophen (APAP) Elderly Polypharmacy Seniors (13% total population) consume: 40% of all prescription drugs 35% of all OTC drugs Average # Rx meds/yr (OTC NOT included) 65-69 yrs: >13 80-84 yrs: ~18 Am. Soc. Consultant Pharmacists 2004 Common Elderly Neurobehavioral Symptoms Balance/gait problems Dizziness Confusion Insomnia Fatigue Irritability Depressed mood Medications & Fall Risk Wolcott et al 2009 Prescribing Cascade Drug treatment of other drug-related side effects increases ADE risk! (particularly when # meds exceeds 10) Major ADE Determinants to Address in Patient Care Inappropriate prescribing* (IP) Drug regimen nonadherence* Unexpected interactions (drugdrug, drug-disease, drug-diet, etc.) *Overuse and/or underuse! IP Occurrence by Type (1989/90) → (1992/93) → Treatment indication? Hanlon et al (2002) Other ADE Factors to Consider Critical transition point (e.g., hospital-to-home) provider and/or patient errors Multiple prescribers per patient Patient-related: ↓ functional status ↓ care support (family, finance) Case 20 yo college student admitted for morning stiffness, unsteady walk, and dysphoria. PMH: bipolar disorder; gastroesophageal reflux disorder (GERD) Medications: Geodon 60 mg BID Wellbutrin SR 150 mg qAM Risperdal 2 mg qHS E-mycin 333 mg TID Case (cont’d) Failed GERD Rx with Reglan due to “muscle stiffness” (parkinsonism?) Relatively high susceptibility to druginduced parkinsonism? Started on GERD therapy (oral erythromycin) about 2 months prior to hospitalization. Pharmacodynamic Determinants? Agonist (+) or Antagonist (- ) Drug Wellbutrin (bupropion) D2 + Geodon (ziprasidone) - - Risperdal (risperidone) - - Direct Adverse Drug Effects? Drug Extrapyramidal Side Effects (EPS)* Wellbutrin No Geodon Maybe Risperdal Maybe Erythromycin No *EPS: dystonia, parkisonism Pharmacokinetic (PK) Factors? Phase I Metabolism - CYP450: Drug 2D6 bupropion ↓ erythromycin 3A4 ↓ PK Interactions of Concern Geodon (ziprasidone) Level Drug 2D6 3A4 bupropion erythromycin PK Interactions of Concern Risperdal (risperidone) Level Drug 2D6 Wellbutrin Erythromycin 3A4 Clinical Effects of Concern Drug EPS Wellbutrin Indirect Geodon Direct Risperdal Direct Erythromycin Indirect* *Straw that broke the camel’s back? Other Effects of Concern? Agonist (+) or Antagonist (- ) Drug Wellbutrin (bupropion) D2 + Geodon (ziprasidone) - - Risperdal (risperidone) - - Orthostatic hypotension ADE Primary Prevention Reduce IP (overuse AND underuse) Increase patient adherence Improve practice safety and clinical outcome Collaborative interdisciplinary approach!!! F.A.M.E.* Trial (2004-06) >65yo army hospital pts on > 4 chronic disorder meds. Intervention “combo”: Pharmacist review and counseling Regular follow-up Use of BP- and lipid-lowering medication blister packs Prospective trial: consecutive ~6-mo. phases: * “Observation” (n = 200) “Randomization” (n = 159) Federal Study of Adherence to Medications in the Elderly Brookes 2007 (Lee et al 2006) Medication Therapy Management (MTM) EMR EMR = electronic medical records Pr Patient Pr = prescriber Ph = pharmacist Ph EPR EPR = electronic pharmacy records Error Prevention Medication Therapy Management (MTM) EMR EMR = electronic medical records Pr Patient Pr = prescriber Ph = pharmacist Ph EPR EPR = electronic pharmacy records Medication Therapy Management (MTM) EMR EMR = electronic medical records Pr Patient Pr = prescriber Ph = pharmacist Ph EPR EPR = electronic pharmacy records Medication Therapy Review “The single most effective and necessary step to ensure appropriate prescribing is to assess all medications prescribed at every visit.” Ballentine 2008 Missing in current practice? SAFE Practice Search for ADE: Symptoms/signs Risk factors (e.g., IP, nonadherence) Address/Avoid: IP (e.g., inappropriate drug, dose, frequency, duration) Automatic refills SAFE Practice Find and apply cost-effective treatment: Simpler/lower-cost regimen Close monitoring (adherence, outcome) Synchronized refills Educate/inform: Patient/family Providers Safe Practice “Rule of Thumb” “Start low, go slow, listen and watch closely!” Patient’s Role More active care partner? In Closing… “As lay people and physicians increase their demands for coherent, evidence-based, unbiased drug information, we would all be well served by a comprehensive program to replace our current patchwork of bad communication and excessive promotion with a responsible national system of balanced, evidence-based, and user-friendly drug information.” Avorn & Shrank 2009 Questions? Comments? References American Society of Consultant Pharmacists. Seniors at risk: designing the system… Available at: http://www.ascp.com/publications/ seniorsatrisk/upload/AtRisk.pdf (accessed 06/21/09) Avorn J, Shrank WH. Communication drug benefits and risks effectively: there must be a better way. Ann Int Med 2009;150(8):563-5. Ballentine NH. Polypharmacy in the elderly: maximizing benefit, minimizing harm. Crit Care Nurs Q 2008;31(1):40-5. Brookes L. Methods to improve adherence: The FAME Trial. 2007. Available at: http://cme.medscape.com/viewarticle/552105 (accessed 06/21/09) Gurwitz JH, Field TS, Harrold LR, Rothschild J, et al. Incidence and Preventability of adverse drug events among older persons in the ambulatory setting. JAMA 2003;289:1107-1116. Hanlon JT, Schmader KE, Koronnkowski MJ, Boult C, Artz MB, et al. Use of inappropriate prescription drugs by older people. J Am Geriatr Soc 2002;50:26-34. References Lee JK, Grace KA, Taylor AJ. Effect of pharmacy care program on medication adherence and persistence, blood pressure and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA 2006;296(21)2563-2571. Wolcott JC, Richardson KJ, Wiens MO, Patel B. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med 2009;169(21):1952-60.