* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download No Slide Title
Victor Skumin wikipedia , lookup
Critical Psychiatry Network wikipedia , lookup
Moral treatment wikipedia , lookup
Anti-psychiatry wikipedia , lookup
Child psychopathology wikipedia , lookup
Cases of political abuse of psychiatry in the Soviet Union wikipedia , lookup
Asperger syndrome wikipedia , lookup
Mentally ill people in United States jails and prisons wikipedia , lookup
Political abuse of psychiatry wikipedia , lookup
Community mental health service wikipedia , lookup
Mental disorder wikipedia , lookup
Mental status examination wikipedia , lookup
Glossary of psychiatry wikipedia , lookup
Psychiatric rehabilitation wikipedia , lookup
Abnormal psychology wikipedia , lookup
Political abuse of psychiatry in Russia wikipedia , lookup
Psychiatric and mental health nursing wikipedia , lookup
Emergency psychiatry wikipedia , lookup
Causes of mental disorders wikipedia , lookup
History of psychiatric institutions wikipedia , lookup
History of psychiatry wikipedia , lookup
Mental health professional wikipedia , lookup
Deinstitutionalisation wikipedia , lookup
Developmental disability wikipedia , lookup
Diagnostic and Statistical Manual of Mental Disorders wikipedia , lookup
Classification of mental disorders wikipedia , lookup
Pyotr Gannushkin wikipedia , lookup
Psychiatric hospital wikipedia , lookup
History of mental disorders wikipedia , lookup
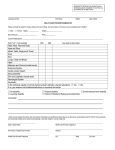
DEVELOPMENTAL DISABILITY AND MENTAL HEALTH: ISSUES IN ASSESSMENT AND MANAGEMENT Dr Seeta Durvasula seetad@med.usyd.edu.au Dr Vivienne Riches vriches@med.usyd.edu.au 7th October 2008 Developmental Disability The term “developmental disability” means a severe, chronic disability of a person which: is attributed to an intellectual, or physical impairment or combination of intellectual and or physical impairment; is manifested before the person attains the age of 18; is likely to continue indefinitely deficits in adaptive behaviour Intellectual disability/ Learning disability Intellectual Disability refers to substantial limitations in present functioning. It is characterized by significantly sub-average intellectual functioning, existing concurrently with related limitations in two or more of the following applicable adaptive skill areas: communication, self care, home living, social skills, community use, self direction, health and safety, functional academics, leisure, and work. Mental retardation manifests before age 18. *AAMR (2002). Mental Retardation: Diagnosis, classification, and systems of support (10th Ed.). Washington, DC:AAMR *Now AAIDD Dual diagnosis Currently between 20% to 35% of all noninstitutionalized persons with intellectual disability are diagnosed as “mentally retarded/mentally ill, compared to 15 to 19%of the general population who meet the criteria of mental illness as defined by the American Psychiatric Association. (American Psychiatric Association, 1995; Einfeld & Tonge, 1991; 1992; Iverson & Fox, 1989; Menolascino & Stark, 1984). Issues that can adversely influence assessment & treatment Diagnostic overshadowing Overemphasis on the intellectual disability at the expense of the psychiatric condition Attention to symptomatology rather than signs (observed behaviour) Additional stigmatization (Luckasson et al, 1992; Reiss, Levitan, & Szysko, 1982). Relevance to general practice Prevalence of ID – 1.8% of population (AIHW, 1998) Increasing life span - 50-60 years Higher risk of physical and mental health problems Majority live in the community with families / supported accommodation Access generic health services Prevalence: mental health problems 41% have a mental health problem Schizophrenia/delusional disorder 3 times higher than in general population Depression Einfeld & Tonge (1996) 3 times higher in people with Down Syndrome Dementia 4 times more common than in general population Types of mental health disorders Same range as in general community Some types of developmental disability associated with specific conditions Down Syndrome - depression, dementia Phenylketonuria - anxiety, depression Prader Willi Syndrome - psychosis, depression Other problem behaviours/challenging behaviours - consider other factors Epilepsy common co-morbid condition Clinical Presentation May be different to that of general population - especially those with severe/profound disability due to: reduced cognitive abilities communication difficulties high prevalence of co-morbidity Some atypical clinical presentations: aggression self injurious behaviour non compliance loss of skills Possible aetiology Organic causes physical illness, pain, effects of medication Psychiatric disorders Behavioural phenotypes e.g. Prader Willi Syndrome Environmental e.g. GORD, middle ear infection, sleep apnoea, psychotropics, lack of choice, change in routine, frustration Life events - grief, loss, abuse Clinical Assessment: history History of behaviour - where, when, precipitants/exacerbating / relieving factors; previous history new or changed behaviour, cyclic patterns accompanying behaviours past medical history / systems review medications: prescription/OTC/alternative functional abilities - esp. communication life circumstances - recent change? family history - medical, psychiatric Clinical Assessment: history For reliability, may need multiple sources: patient if possible simple short sentences, start with open-ended questions family member / friend formal carer/s other support people - day placement, respite care health records behaviour observation chart Behavioural measures Checklists eg. DASS 21; DBC Reports, files, Observational data eg. A-B-C Antecedents Behaviour Consequences Sample Behaviour Chart Clinical Assessment: examination/ investigations Full physical examination Mental state examination Investigations - as indicated consider vision/hearing assessments thyroid function tests Management Often need multidisciplinary approach Treat physical disorders May need to review medication Refer/ treat psychiatric disorders Address environmental issues e.g psychologist, psychiatrist, speech therapist structure, consistency Effective communication methods Counselling and social support MONITOR AND REVIEW How to make the consultation work Good planning is essential plan long consultation insist on all records accompanying patient request carer with knowledge of patient to accompany may need more than one consultation to obtain all information from variety of sources Give explicit written instructions/information especially for prn medications Working with formal caregivers Issues high turnover of staff frequent use of casual staff range of knowledge / experience / skills incomplete information often given record keeping Psychotropic medication: principles Comprehensive assessment first Where possible, treat the underlying condition, don’t merely suppress the behaviour Consider non-pharmacological treatment options Medication is seldom the sole solution - other therapeutic modalities may be required avoid using medication as a restraint behavioural intervention, counselling, environmental changes Baseline observations and reliable documentation of response to Rx is vital : checklists, rating scales Psychotropic medication: principles Continue medication only if documented improvement Response to medication may be idiosyncratic - start with small doses and watch for side effects Consider reducing dose if symptoms absent for reasonable period reduce slowly / may need extra support at this time monitor and document response Adapted from: Einfeld SL “Guidelines for the use of psychotropic medication in individuals with developmental disabilities” Australia and New Zealand Journal of Developmental Disabilities, 1990 16(1):71-73 Psychotropic medication:side effects More vulnerable to CNS side effects S/E can be missed/misinterpreted: tardive dyskinesia may be mistaken for stereotypic behaviour akathisia can be misdiagnosed as anxiety and neuroleptic dose increased Beware paradoxical response to benzodiazepines increased agitation Seizure threshold lowered by some neuroleptics/antidepressants Issues to consider Beware of “diagnostic overshadowing” Consider psychiatric disorders Communication difficulties Acquiescence/ nay saying Functional aspect of behaviour ask about appetite, sleep patterns, tearfulness, hallucinations, delusions attention seeking, protesting, escaping Consent to treatment Resources Local DADHC office Local mental health service Statewide Behaviour Intervention Service (SBIS) : Ph: (02) 8876 4000 Private practitioners eg psychologists, psychiatrists, speech pathologists NSW Developmental Disability Health Unit Ph: (02) 9808 9287 Brain & Mind Research Institute (University of Sydney) Ph: (02) 9351 0799 www.bmri.org.au/cc_ptfmly.html Summary High prevalence of mental health problems in people with developmental disability Beware of “diagnostic overshadowing” Consider physical, psychiatric, psychological and environmental factors Multiple approaches to management are required - medical, behavioural, environmental, social Case Scenario A Michael, 42 yrs Down Syndrome, mild level of ID Lives in group home “Not himself” for last 3 months losing skills- e.g. self care, independent travel work placement threatened - slow, forgetful not interested in social activities irritable, aggressive Case Scenario A … Wears glasses for myopia On thioridazine for “behavioural problems” started 10 years ago, after moving into group home Father died of MI 18 months ago Case worker recently changed jobs Case Scenario A : differential diagnosis Sensory impairment vision hearing Hypothyroidism Depression Neuroleptic induced symptoms Alzheimer’s Disease Case Scenario B Phillip - 32 year old man Down Syndrome – moderate intellectual disability Lives with mother, older siblings moved out Works 2 days per week supported employment –fast food outlet Psychiatrist treating for schizophrenia past two years Slowed performance, loss of skills Reduced communication Aggressive behaviour – shouting at neighbour – unknown provocation Talking to imaginary people Case Scenario B …. Falling asleep in waiting room 9am Father died when child – left taped message which Phillip listens to regularly Grandmother died 2 years previously Case Scenario B : differential diagnosis Behaviour of concern – aggression Depression Schizophrenia Fantasy Grief