* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download No Slide Title
Survey
Document related concepts
Transcript
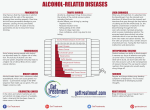
Medical Nutrition Therapy for Liver, Biliary System, and Exocrine Pancreas Disorders © 2004, 2002 Elsevier Inc. All rights reserved. Relationship of Organs of the Upper Abdomen A, Liver (retracted upward); B, gallbladder; C, esophageal opening of the stomach; D, stomach (shown in dotted outline); E, common bile duct; F, duodenum; G, pancreas and pancreatic duct; H, spleen; I, kidneys. Courtesy The Cleveland Clinic Foundation, Cleveland, Ohio, 2002. The Liver Largest gland in the body (about 1500 g) Essential for life, though survival is possible with 10-20% function Plays major role in macronutrient and micronutrient digestion, metabolism, and storage Metabolizes steroids, detoxifies drugs, alcohol, ammonia Diseases of the Liver Acute viral hepatitis Fulminant hepatitis Chronic hepatitis Alcoholic liver disease, alcoholic hepatitis, and cirrhosis Non-alcoholic hepatic steatosis (NASH) Diseases of the Liver Cholestatic liver diseases —Primary biliary cirrhosis —Sclerosing cholangitis Inherited disorders Other liver diseases Acute Viral Hepatitis Widespread inflammation of the liver that is caused by hepatitis viruses A, B, C, D and E – Hep A: oral-fecal route – Hep B and C: body fluids – Hep D: occurs only in pts with Hep B – Hep E: oral-fecal route; seen more often in Asia, Africa, Mexico Hasse JM et al. ASPEN Nutrition Support Practice Manual, 2nd edition, 2005 Acute Viral Hepatitis Four phases of symptoms: 1. Prodromal phase 2. Preicteric phase 3. Icteric phase 4. Convalescent phase Risk Factors for Chronic Viral Hepatitis Injection drug use Chronic hemodialysis Blood transfusion or transplantation prior to 1992 (HCV) Receipt of blood (including needlestick) from a donor subsequently testing positive for HCV Risk Factors for Chronic Viral Hepatitis Receipt of clotting factor concentrates produced before 1987 Asian ancestry (HBV) Unvaccinated health care workers Birth to mother with chronic HBV or HCV Possible Risk Factors Body piercing or tattooing Multiple sexual partners or sexually transmitted diseases Health care workers (HCV) Contacts of HCV positive persons Source: NACB Laboratory Guidelines for Screening, Diagnosis, and Monitoring of Hepatic Injury. Dufour, Lott, Nolte, Gretch, Koff, Seeff Fulminant Hepatitis Syndrome in which severe liver dysfunction is accompanied by hepatic encephalopathy within 8 weeks Causes include viral hepatitis (75%), chemical toxicity (acetaminophen, drug reactions, poisonous mushrooms, other poisons) Complications include cerebral edema, coagulopathy, bleeding, cardiovascular complications, renal failure, pancreatitis Chronic Hepatitis At least 6-month course of hepatitis or biochemical and clinical evidence of liver disease with confirmatory biopsy findings of unresolving hepatic inflammation Can be caused by autoimmune, viral, metabolic, or toxic etiologies Alcoholic Liver Disease: Most Common Liver Disease Alcohol excess and abuse Most common cause of liver disease in the U.S. Fourth leading cause of death among middle-aged Americans Alcohol problems are highest among young adults, ages 18 to 29. Stages of Alcoholic Liver Disease Hepatic steatosis Alcoholic hepatitis Alcoholic (Leannec’s) cirrhosis Alcoholic Liver Disease Disease resulting from excessive alcohol ingestion characterized by fatty liver (hepatic steatosis), hepatitis, or cirrhosis Most common liver disease in the U.S., except perhaps fatty liver secondary to obesity Toxic Effects of Excess Alcohol Use © 2004, 2002 Elsevier Inc. All rights reserved. Alcoholic Liver Disease Metabolic Changes Steatorrhea Wernicke-Korsakoff syndrome Peripheral neuropathy Pellagrous psychosis Folate deficiency End-Stage Alcoholic Liver Disease Possible Characteristics Malnutrition Portal hypertension with varices Ascites Hyponatremia Hepatic encephalopathy Glucose alterations End-Stage Alcoholic Liver Disease Possible Characteristics Fat malabsorption Osteopenia Thrombocytopenia with anemia Non-Alcoholic Steatohepatitis (NASH) Histologically resembles alcoholic hepatitis Most common cause of chronic hepatic injury other than viruses and alcohol; most common cause of cryptogenic cirrhosis Commonly in middle-aged women with obesity and/or diabetes but appears in persons without these risk factors Non-Alcoholic Steatohepatitis (NASH) Patients with NASH often have abnormal lipid profiles Differs from alcoholic hepatitis in that ALT is higher than AST except in cirrhosis Weight loss may cause significant improvement in enzyme results; in one study a 1% reduction in weight caused an average fall of 8.1% in ALT Biopsy is the only diagnostic procedure with adequate specificity Cholestatic Liver Diseases Primary biliary cirrhosis (PBC) An immune-mediated chronic cirrhosis of the liver due to obstruction or infection of the small and intermediate-sized intrahepatic bile ducts, whereas the extrahepatic biliary tree and larger intrahepatic ducts are normal 90% of patients are women Cholestatic Liver Diseases Sclerosing cholangitis Fibrosing inflammation of segments of extrahepatic bile ducts, with or without involvement of intrahepatic ducts May be an immune disorder 50-75% of patients also have inflammatory bowel disease 60-70% are men Cholestatic Liver Diseases Sclerosing Cholangitis Increased risk of fat soluble vitamin deficiencies due to steatorrhea Hepatic osteodystrophy due to vitamin D and calcium malabsorption resulting in secondary hyperparathyroidism and osteomalacia or rickets Treated with immunosuppressants Inherited Disorders: Hemochromatosis Inherited disease of iron overload Store 20-40 g of iron in the liver compared with .3 to .8 g in normal persons Causes hepatomegaly, esophageal varices, glucose intolerance Treated by phlebotomy Inherited Disorders: Wilson’s Disease Autosomal recessive disorder associated with impaired biliary copper excretion Copper accumulates in liver, brain, cornea, and kidneys May present with neurological signs, KayserFleischer rings, low serum ceruloplasmin, psychiatric symptoms Always presents before age 40 Treated with copper-chelating agents, zinc supplementation, low copper diet Inherited Disorders: α1-antitrypsin deficiency Causes cholestasis or cirrhosis and can cause liver and lung cancer No treatment but liver transplant Other Liver Diseases Liver tumors Systemic diseases (rheumatoid arthritis, systemic sclerosis) Nonalcoholic steatohepatitis** Acute ischemic and chronic congestive hepatopathy Parasitic, bacterial, fungal, and granulomatous liver diseases Normal Liver vs. Damaged Liver Microscopic Image of (A) Normal Liver; (B) cirrhotic liver) (Adapted from Bray GA. Gray DS, Obesity, part 1: Pathogenisis. West J Med 149:429, 1988; and Lew EA, Garfinkle L; Variations in mortality (From Kanel by weight G, Korula among J. Atlas 750,000 of Liver menPathology. and women. W.B. J Clin Saunders, Epidemiol 1992.) 32:563, 1979.) © 2004, 2002 Elsevier Inc. All rights reserved. Clinical Manifestations of Cirrhosis © 2004, 2002 Elsevier Inc. All rights reserved. Interpretation of Lab Data In Liver Disease Liver Test Panel Aspartate transaminase (AST) Alanine aminotransferase (ALT) Alkaline phosphatase (ALP) Total bilirubin Direct bilirubin PT/PTT Ceruloplasmin Total protein Albumin Viral serologies AST and ALT Enzymes released into circulation following injury or death of cells in heart, liver, lungs, and other parts of the body High AST (200 U/L) and ALT (300 U/L) are indicative of liver disease in presence of jaundice or nonspecific symptoms of acute illness Levels are higher in acute hepatic injury; lower in uncomplicated hepatitis and chronic liver disease Transaminases relate more to cause of liver injury than prognosis ALP (alkaline phosphatase) Usually normal in acute and chronic liver disease High levels are usually indicative of obstruction of biliary drainage Bilirubin Results from the breakdown of hemoglobin in the red blood cells and removal from the body by the liver, which excretes it in bile Rises when the liver is unable to excrete bilirubin or when there is excessive destruction of red blood cells In viral hepatitis, total bilirubin >257 micromoles/L indicates severe liver injury In alcoholic hepatitis, bilirubin >428 micromoles/L predicts high likelihood of death Two Forms of Bilirubin Indirect or unconjugated bilirubin: is protein bound; with increased destruction of red blood cells Direct or conjugated bilirubin: not protein bound; circulates until it reaches the liver, where it is conjugated; in dysfunction or blockage of the liver Dx: first, measure total bilirubin; if that is high, measure direct and indirect Reference values: Total: 0.3-1.0 mg/dL, or 5-17 micromoles/L Conjugated: 0.0-0.2 mg/dL or 0.0-3.4 micromoles/L Bilirubin Circulation Hepatocellular Jaundice direct (conj) bilirubin Injury or disease of the parenchymal cells of the liver caused by Viral hepatitis Cirrhosis Infectious mononucleosis Reactions of certain drugs such as chlorpromazine Obstructive Jaundice Direct bilirubin Obstruction of the common bile or hepatic ducts due to stones or neoplasms. Causes high conjugated bilirubin levels due to bile regurgitation Hemolytic Jaundice unconjugated bilirubin Overproduction of bilirubin resulting from hemolytic processes After blood transfusions Pernicious anemia Sickle cell anemia Transfusion reactions Ceruloplasmin Normal value: 25-63 mg/dL (250-630 mg/L) Copper bound to ceruloplasmin constitutes the largest amount of Cu2+ in circulation In Wilson’s disease Cu2+ mobilization from the liver is drastically reduced because of low production of ceruloplasmin Values <14 mg/dL may be expected However, low ceruloplasmin is not the primary defect in Wilson’s disease; some patients with Wilson’s are not low Screening for Liver Disease Asymptomatic high risk individuals should be screened for chronic hepatitis ALT is the most cost-effective screening test for metabolic or drug-induced liver injury AST should also be measured with hx of alcohol abuse (in alcoholic hepatitis AST is > ALT) Individuals at high risk for viral hepatitis should be screened using specific viral serologies (HBsAg, anti-HCV, IgM anti-HAV, anti-HBS, HCV-RNA) in addition to ALT Predictors of Prognosis Prothrombin time: the most important predictor of prognosis; prolonged PTT indicative of poor prognosis Albumin: serum albumin <2.5 g/dL indicates high risk of death Lab Tests in Acute Liver Disease Disease Peak ALT (x URL)* AST/Alt Ratio Peak Bili (mg/dL) Viral hepatitis 10-40 <1 <15 PTT Prolongati on (s) <3 Alcoholic hepatitis Toxic injury 2-8 >2 <15 1-3 >40 >1 early <5 >5 transient Ischemic injury >40 >1 early <5 >5 transient *upper reference limit Source: NACB Laboratory guidelines for screening, diagnosis, and monitoring of hepatic injury. Dufour, Lou, Nolic, Gretch, Koff, Seeff Causes of Elevated ALT and/or AST Cause Key Feature Screening test Confirming test Non-alcoholic steatohepatitis (NASH) Most common cause other than viral, alcoholic None biopsy Hemochromatosis Autosomal recessive trait 1:200 among northern European ancestry Transferrin saturation >45% HFE gene analysis for C282Y mutation Source: NACB Laboratory guidelines for screening, diagnosis, and monitoring of hepatic injury. Dufour, Lou, Nolic, Gretch, Koff, Seeff Causes of Elevated ALT and/or AST Cause Wilson’s Disease Autoimmune hepatitis Key Feature Screening test Autosomal Low cerulorecessive trait. plasmin in 1:30,000 65-95% individuals; homozyhemolytic gous; 20% anemia, renal heterozyinjury gotes Up to 18% of ANA and non-viral ASMA; false hepatitis; mainly positive young women anti-HCV common Confirming test Genetic analysis, low serum copper, high urine copper Biopsy Causes of Elevated ALT and/or AST Cause Key Feature Primary biliary cirrhosis Middle aged women; mainly ALP; often associated with Sjogren’s Syndrome Schlerosing Young to middle cholangitis aged men; mainly ALP; often with IBD Screening test Anti-mitochondrial antibody Confirming test Biopsy Anti neutrophil cytoplasmic antibodies; ASMA, ANA may be + Bile duct imaging Interpretation of Nutrition Assessment Tests in Patients with End-Stage Liver Disease Body weight Anthropometric measurements Creatinine-height index Nitrogen balance studies Visceral protein levels Immune function tests SGA Parameters for Nutritional Evaluation of Liver Transplant Candidates History – Weight change (fluid changes) – Appetite – Taste changes and early satiety – Dietary recall (calories, protein, sodium) – Persistent gastrointestinal problems (nausea, vomiting, diarrhea, constipation, difficulty chewing or swallowing) SGA Parameters for Nutritional Evaluation of Liver Transplant Candidates Physical – Muscle wasting – Fat stores – Ascites or edema Existing conditions – Disease state and other problems that could influence nutritional stores such as hepatic encephalopathy, GI bleeding, renal insufficiency, infection SGA Parameters for Nutritional Evaluation of Liver Transplant Candidates Nutritional rating (based on results of above parameters) – Well nourished – Moderately malnourished – Severely malnourished Malnutrition and Ascites in End Stage Liver Disease Clinical Manifestations of Cirrhosis © 2004, 2002 Elsevier Inc. All rights reserved. Esophageal Varices Causes of Malnutrition in Liver Disease Anorexia Early satiety or dysgeusia Nausea and vomiting Maldigestion or malabsorption Restricted diets Altered metabolism Malnutrition in Liver Disease— Pathophysiology Algorithm content developed by John Anderson, PhD, and Sanford C. Garner, PhD, 2000. Updated by Jeanette M. Hasse and Laura E. Matarese, 2002. Malnutrition in Liver Disease— Medical and Nutritional Management Algorithm content developed by John Anderson, PhD, and Sanford C. Garner, PhD, 2000. Updated by Jeanette M. Hasse and Laura E. Matarese, 2002. Vitamin/Mineral Deficits* in Severe Hepatic Failure Vitamin Vitamin Vitamin Vitamin Vitamin Vitamin Folate A D E K B6 B12 Niacin Thiamin Zinc Magnesium Iron Potassium Phosphorus * May be related to fat malabsorption, medications, alcoholism (p. 752 Krause) Four Stages of Hepatic Encephalopathy Stage I II Symptom Mild confusion, agitation, irritability, sleep disturbance, decreased attention Lethargy, disorientation, inappropriate behavior, drowsiness III Somnolence but arousable, incomprehensible speech, confusion, aggression when awake IV Coma End-Stage Liver Disease Hepatic Encephalopathy 1. Consider major causes of encephalopathy • GI bleeding • Fluid and electrolyte abnormalities • Uremia • Use of sedatives • Hypo- or hyperglycemia • Alcohol withdrawal • Constipation • Acidosis End-Stage Liver Disease Hepatic Encephalopathy—cont’d 2. Treat underlying cause. 3. Treat with medications. • Lactulose • Neomycin 4. Ensure adequate diet is consumed. MNT in End-Stage Liver Disease Energy needs are highly variable; 30% of pts are hypometabolic and 20% hypermetabolic Use indirect calorimetry where available Energy: 25 to 30 kcal/kg dry weight Ascites increases REE by 10% Hasse et al. ASPEN Nutrition Support Practice Manual, 2nd Edition, 2005, p. 238 End-Stage Liver Disease Fat: 25% to 40% of kcal May try MCT if steatorrhea is present; with severe case, try fat restriction and discontinue if diarrhea does not improve Protein: 1 to 1.5 g/kg dry wt depending on degree of malnutrition, malabsorption, metabolic stress End-Stage Liver Disease— cont’d May try BCAA formulas for >grade 2 encephalopathy CHO: high intake of both complex and simple carbohydrates Vitamin and mineral supplements Electrolytes: restrict sodium with edema or ascites (1500-2000 mg/day) Fluid: restrict fluid if hyponatremia is present 1000-1500 mL Hasse. ASPEN Nutrition Support Practice Manual, 2nd edition, 2500, p. 239 Amino Acids Commonly Altered in Liver Disease *=essential) Aromatic amino acids—serum levels increased —Tyrosine —Phenylalanine* —Free tryptophan* Branched-chain amino acids—serum levels decreased —Valine* —Leucine* —Isoleucine* Other amino acids—serum levels increased —Asparagine —Methionine* —Histidine* —Glutamine Esophageal Varices MNT for Esophageal Varices Endoscopic tube used to tamponade bleeding vessels Repeated therapy may cause esophageal strictures, dysphagia Cannot feed enterally during acute bleeding episodes May require PN if patient unable to eat MNT for Ascites Ascites is accumulation of fluid in the abdominal cavity Caused by portal hypertension, hypoalbuminemia, lymphatic obstruction, renal retention of sodium and fluid Medical treatment: paracentesis, diuretics MNT: restrict sodium to 2 grams or less More severe restrictions may be unpalatable MNT: supplement protein if frequent paracentesis MNT for Hyponatremia Occurs because of decreased ability to excrete water because of persistent release of antidiuretic hormone, sodium loss via paracentesis, excessive diuretic use, sodium restriction Fluid intake restricted to 1 to 1.5 liter per day (as low as 500-750 + urinary loss) Moderate sodium intake Hepatic Encephalopathy Can be caused by GI bleeding, fluid/electrolyte abnormalities, uremia, infection, blood glucose derangements, alcohol withdrawal Occurs in 50-70% of pts with chronic hepatic failure Caused by protein in only 5% 95% of persons with cirrhosis tolerate mixed protein diets of up to 1.5 g/kg Hasse ASPEN Nutrition Support Practice Manual, 2nd edition, p. 236 Hepatic Encephalopathy: Medical Treatment Neomycin or lactulose Lactulose: nonabsorbable disaccharide. Acidifies colonic contents, acts as laxative to excrete ammonia Neomycin is nonabsorbable antibiotic that decreases colonic ammonia production Hepatic Encephalopathy: Medical Treatment Identify and treat acute causes, e.g. Variceal bleed Infection Electrolyte imbalance Sedatives Constipation Hasse JM et al. ASPEN Nutrition Support Practice Manual, 2nd Edition, 2005 Hepatic Encephalopathy: MNT Role of protein in encephalopathy controversial Encephalopathy may be caused by imbalance of aromatic and branched chain amino acids Protein restriction not proven to improve mental state Supplements enriched in BCAA, low in AAA may help Hepatic Encephalopathy: MNT If patient is protein sensitive, start with .5 to .7 g protein/kg and increase level to tolerance, up to 1.5 g/kg in protein-calorie malnutrition Provide adequate calories to prevent catabolism of endogenous protein stores Glucose Derangements Glucose intolerance in nearly 2/3 of patients with cirrhosis (10-37% develop diabetes) Occurs because of insulin resistance in peripheral tissues Hyperinsulinemia, possibly because insulin production increased, hepatic clearance decreased Fasting hypoglycemia d/t decreased glycogen stores; pts may need small, frequent meals Steatorrhea Replace LCT with MCT oils (in some nutrition supplements or as oil) May trial low fat diet, but do not restrict unnecessarily; if steatorrhea doesn’t improve, discontinue restriction Nutrition Care Guidelines for Liver Transplantation Pretransplantation Immediate posttransplantation Long-term posttransplantation Calories Protein Fat Carbohydrate Sodium Fluid Calcium Vitamins Medications* Commonly Used after Liver Tx Azathioprine Antithymocyte globulin Basiliximab Cyclosporine Daclizumab Glucocorticoids Muromonab-CD3 Mycophenolate mofetil Sirolimus Tacrolimus 15deoxysperagualin *Most have drug-nutrition interactions. See p. 756 Krause Liver Transplantation— Diet Nutrition support: pre- and posttransplant Long-term preventive nutrition to optimize health and to avoid or minimize —Excessive weight gain —Hyperlipidemia —Hyperglycemia —Hypertension —Osteopenia CAM in Liver Disease Milk Thistle (silymarin) – purported anti-hepatotoxic and anti-inflammatory activity Scientific evidence is mixed CAM in Liver Dx: Potentially Hepatotoxic Products Borage Chaparral Coltsfoot Comfrey DHEA Germander Jin bu huan Kava kava Liferoot Pennyroyal Periwinkle Poke root Skullcap (American) Shark cartilage Hasse JM. ASPEN Nutrition Support Practice Manual, 2nd Edition, 2005. Summary Liver disorders—role of liver is so crucial to overall health, its destruction is quite serious Goals—support maintenance of as much normal liver function as possible Transplantation, if needed Relationship of Organs of the Upper Abdomen A, Liver (retracted upward); B, gallbladder; C, esophageal opening of the stomach; D, stomach (shown in dotted outline); E, common bile duct; F, duodenum; G, pancreas and pancreatic duct; H, spleen; I, kidneys. Courtesy The Cleveland Clinic Foundation, Cleveland, Ohio, 2002. Functions of the Gallbladder Primary function is to concentrate, store, excrete bile (produced by the liver) Bile: primary constituents are cholesterol, bilirubin (from hemoglobin) and bile salts Bile salts are essential for digestion and absorption of fats, fat soluble vitamins, some minerals Gallbladder and pancreas use common duct to release digestive juices into duodenum Diseases of liver, pancreas, and gallbladder interrelated Diseases of the Gallbladder: Cholelithiasis Calculi form in the gallbladder Choledocholithiasis: stones slip into bile ducts, obstruction, pain, cramps Blockage can cause cholecystitis, impaired lipid absorption, light colored stools; secondary biliary cirrhosis; obstruction of the distal common bile duct can lead to pancreatitis if pancreatic duct is blocked Choledocholithiasis http://www.nlm.nih.gov/medlineplus/ency/images/ency/fullsize/17038.jpg Choledocholithiasis Affects millions of Americans each year; many asymptomatic Risk factors are female gender, pregnancy, older age, family history, obesity, truncal body fat distribution, diabetes, certain drugs (lipid lowering meds, oral contraceptives, estrogens) Rapid weight loss (gastric bypass, fasting, VLC diets) associated with biliary sludge and gallstones Choledocholithiasis Medical Mgt Surgical removal of the gallbladder via open lap or laparoscopic procedure Chemical dissolution or shock wave lithotripsy may be tried Stones in bile ducts may be removed via endoscopic retrograde cholangiopancreatography techniques (ERCP) Cholelithiasis MNT Correct risk factors if possible (obesity and VLC diets) Cholecystitis: low fat diet to prevent gallbladder contractions After cholecystectomy, diet can be advanced to regular diet as tolerated Liver secretes bile directly into small intestine; intestine adapts Cholecystitis MNT Acute: NPO initially. Use PN if prolonged. Then initiate low fat diet (hydrolyzed lowfat enteral feeding or oral diet with 30-45 g fat/day) Chronic: long term low fat diet (2530% of calories May need water-soluble forms of fatsoluble vitamins if malabsorption is suspected Functions of the Pancreas Endocrine Functions: secretes glucagon, insulin, somatostatin into bloodstream for regulation of glucose Exocrine Functions: secretes enzymes directly into GI tract to digest protein, fat, carbohydrate Factors that Govern Pancreatic Secretions Cephalic phase: mediated through the vagus nerve, initiated by the sight, smell, taste and anticipation of food: bicarbonate and pancreatic enzymes Gastric phase: caused by gastric distention with food; enzyme secretion Intestinal phase: most potent effect, mediated by the release of cholecystokinin Pancreatitis Inflammation of the pancreas, mild or severe Significant morbidity/mortality Symptoms: continuous or intermittent pain of varying intensity to severe upper abdominal pain, radiating to back Symptoms may worsen with ingestion of food Nausea, vomiting, abdominal distention, steatorrhea Elevated serum amylase or lipase; however amylase is nonspecific for pancreatitits Pancreatitis: Causes Chronic alcoholism (most common cause of acute and chronic pancreatitis) Gallstones (a common cause of acute pancreatitis) Trauma, certain drugs Hypertriglyceridemia Hypercalcemia Some viral infections Pancreatitis: Diagnosis Tests of pancreatic function – Secretin stimulation test: measures pancreatic secretion of bicarbonate in response to secretin – Glucose tolerance test: measures endocrine function – 72-hour stool fat test: measures fat absorption that reflects pancreatic lipase secretion Ranson’s Criteria At admission or diagnosis Age >55 years White blood count >16,000 m3 Blood glucose level >200 mg/dl Lactic dehydrogenase >350 IU/L Aspartate transaminase >240 U/L Ranson’s Criteria During first 48 hours Hematocrit decrease of >10 mg/dL Blood urea nitrogen increase of >5 mg/dl Arterial PO2 <60 mmHg Base deficit >4 mEq/L Fluid sequestration >6000 ml Serum calcium level <8 mg/dL Pancreatitis http://www.pennhealth.com/health_info/Surgery/pancreatitis_2.html Acute Hemorrhagic Pancreatitis http://www.pathguy.com/~lulo/lulo0028.htm Acute Pancreatitis 75% alcohol related 15% related to gallstones 10% trauma, hyperlipidemia, hypercalcemia, medications, etc. Mascarenhas et al. ASPEN Nutrition Support Practice Manual, 2nd edition, 2005, p. 211 Energy Needs in Acute Pancreatitis Metabolic stress state: Resting energy expenditure as high as 139% of Harris-Benedict Sepsis may increase energy needs an additional 15% Acute patients more hypermetabolic than chronic patients Mascarenhas et al. ASPEN Nutrition Support Practice Manual, 2nd edition, 2005, p. 211 Nutritional Alterations in Acute Pancreatitis Glucose intolerance in 40 to 90% of patients, caused by stress response, impaired Beta-cell function, and insulin resistance Changes in fat metabolism in 12-15% of patients, primarily steatorrhea and hypertriglyceridemia Nutritional Alterations in Acute Pancreatitis Hypocalcemia in 25% of patients due to ↓ parathyroid hormone secretion, increased calcitonin, hypomagnesemia, hypoalbuminemia, saponification of calcium Ethanol abuse → hypomagnesemia, decreased zinc, thiamine and folate deficiencies Mascarenhas et al ASPEN Nutrition Support Practice Manual, 2005, p. 211 Pancreatic Disorders: Medical Mgt Acute Withhold oral feeding Give IV fluids Administer H2-receptor antagonists, somatostatin Chronic Manage intestinal pH with antacids, H2 receptor antagonists, proton pump inhibitors Administer insulin for glucose intolerance Pancreatitis: MNT Acute Withhold oral feeding Support with IV fluids If oral nutrition cannot be initiated in 57 days, start nutrition support Pancreatitis: Enteral Nutrition Enteral nutrition can be used while resting the pancreas Early enteral feeding may exacerbate symptoms (21% of patients in one case series) Feeding below the ligament of Treitz invokes fewer stimulatory factors Use of elemental low fat formulas is less stimulating than polymeric, higher fat formulas Mascarenhas et al ASPEN Nutrition Support Practice Manual, 2005, p. 211 Pancreatitis: Enteral Recommendations Place nasoenteric tube below the ligament of Treitz Begin infusion with a standard enteral formula If there is concern about a particular patient, a low-fat elemental or peptide formula should be used Monitor patient for intolerance (N/V, abdominal pain, fever, ↑ amylase/lipase PN may be initiated if patient does not tolerate EN Pancreatitis: Enteral Nutrition Stimulation of the GI tract at lower levels may be beneficial EN maintains gut integrity and stimulates blood flow to the gut May preserve immune function and reduce inflammatory response Mascarenhas et al ASPEN Nutrition Support Practice Manual, 2005, p. 211 Pancreatitis: PN Acute (cont) If enteral feedings are not tolerated, PN should be initiated – If TGs are <400 mg/dl use 3-in-1 solution and monitor TG levels – If TGs are elevated (>400 mg/dl) use a dextrose-based solution, monitor serum glucose frequently, and treat as needed with insulin Mascarenhas et al ASPEN Nutrition Support Practice Manual, 2005, p. 211 Pancreatitis MNT Acute Energy needs: AP patients are hypermetabolic and catabolic HB BEE X activity factor X stress factor of 30-50% Protein needs: 1.4-2 g/kg body weight Fat up to 2 g/kg/BW/day; monitor TG Wall-Alonso, Sullivan, Byrne. In Gottslich and Matarese. Contemporary Nutrition Support Practice, p. 434-425. Philadelphia: Saunders, 2003. Pancreatitis: MNT Acute (cont) Once oral diet is started, provide – Easily digested foods – Low fat diet – 6 small meals – Adequate protein intake – Increased calories Pancreatitis: MNT Chronic Provide oral diet as in acute phase TF can be used when oral diet is inadequate Supplement pancreatic enzymes Supplement fat-soluble vitamins and vitamin B12 MNT for Chronic Pancreatitis: Pancreatic Enzymes When pancreatic function diminished by about 90%, malabsorption of protein and fat becomes a problem Avoid large high fat meals and alcohol Pancreatic enzyme replacements given orally with meals (at least 30,000 IU lipase with each meal) Level of fat in the diet should be the most pt can tolerate without steatorrhea or pain May substitute some fat with MCT Whipple Procedure Pancreaticoduodenectomy: often done for pancreatic carcinoma Cholecystectomy, vagotomy, or partial gastrectomy may also be done Pancreatic duct renanastamosed to the jejunum MNT: similar to chronic pancreatitis Whipple Procedure Source: Johns Hopkins http://www.hopkins-gi.org/pages/latin/templates/ index.cfm?pg=disease3&organ=4&disease =24&lang_id=1&pagetype=12&pagenum=263 MNT in Liver/Biliary Disease Disease of the liver/biliary tract has a profound effect on digestion and absorption Often leads to malnutrition; malnutrition exacerbates effect of disease Appropriate nutrition care is key in reducing associated morbidity and mortality and improving quality of life