* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Chapter 9 Homeostasis
Survey
Document related concepts
Transcript
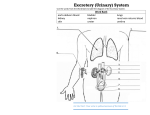
Homeostasis Chapter 9 http://www.bbc.co.uk/schools/gcsebitesize/science/add_aqa_pre_2011/homeo/homeosts.shtml Homeostasis Physiological state of the body Internal physical and chemical conditions are maintained within a tolerable range Includes Temperature, hormone levels, pH, pressure, concentrations of glucose and other solutes in the blood Internal Environment Extracellular fluid Interstitial fluid – fills the spaces between cells and tissues (e.g. plasma) Consists of water, sugars, salts, FA, AA, coenzymes, hormones, neurotransmitters, waster products Regulates flow of chemicals and allows cells to function properly Lymphatic system transports fluid throughout the body Internal Environments Changes in Extracellular Fluid has negative effects on cellular function Body uses organ systems to regulate internal conditions Nervous system Endocrine system Muscular system Integumentary system Excretory system Reproductive system Nervous System Brain, spinal cord, peripheral nerves, sensory organs Receives sensory data from the environment Informs body of external conditions Transmits signals throughout the body Endocrine System Pituitary, thyroid, pancreas, adrenal (glands) Regulates levels of hormones and other chemicals Excretory System Kidneys, bladder, urethra, ureters Rids the body of waste Maintains clean internal environment Integumentary System Skin, sweat glands, hair, nails Maintains a constant body temperature Immune System White blood cells Protects/fights infection Digestive System Liver Breaks down amino acids Detoxifies harmful chemicals (alcohol) Manufactures important proteins Homeostatic Mechanisms Respond to internal and external conditions Feedback systems – Positive/Negative Help bring the body back into balance Breathing rate, heart rate, internal temperature, blood glucose levels Negative Feedback Reduces the output or activity of an organ or system back to its normal range Include 3 elements Sensor Integrator - hypothalamus tissues or organs - detects change control centre – compares conditions from environment with to optimal conditions in the body Set points – ranges of values which need to be maintained Effector returns measured condition back to set point – response Antagnositc effectors – produce opposite effect of change detected Hypothalamus Body’s thermostat Maintains body temperature Optimal body temperature – 35⁰ - 37.8⁰ Body temp falls → vasoconstriction in skin/shivering→ reduced blood flow→ less thermal energy lost to environment → body temp increases Body temp rises → blood vessels dilate/induce vasodilation/sweating → increase blood flow→ increase thermal energy loss to environment→ body temp decreases Signals from hypothalamus make us aware of our own temperature Positive Feedback Mechanisms Increases change in environmental condition Does not result in homeostasis Cause system to become unstable “fight or flight” response reproduction fever Positive feedback mechanisms operate within negative feedback mechanisms Allows body to be brought back into balance Thermoregulation Internal temperature regulation Negative feedback mechanism Thermoreceptors – compare external temp with internal set point Trigger responses (2) Rate of exothermic reactions in body (metabolism) Rate of thermal energy exchange through surface of body Mechanisms of Thermal Energy Exchange Occurs at the surface where body comes into contact with the external environment Exchange of thermal energy occurs through 1 of 4 mechanisms Conduction Convection Radiation Evaporation All of these mechanisms act simultaneously Conduction Flow of thermal energy between molecules that are in direct contact Convection Transfer of thermal energy within a fluid (liquid or gas) Radiation Thermal energy is transferred electromagnetically Evaporation Absorbs thermal energy from skin via water/sweat Homeotherms Animals that maintain a stable internal temperature regardless of external conditions Includes Poikilotherms Endotherms Ectotherms Poikilotherms Fish, amphibians, reptiles, and most invertebrates Body temperature varies with and often matches the temperature of the external environment Endotherms Warm blooded animals (mammals, birds) Homeotherms that use internal physiological mechanisms (metabolism) to generate thermal energy and maintain body temp Remain fully active over a wide range of temperatures Need a constant supply of energy Ectotherms Cold blooded animals (reptiles, amphibians, fish) Homeotherms that use external sources of energy to absorb thermal energy and regulate body temperature Temperature fluctuates with environmental temperature Inactive when temp are too low Undergo thermal acclimatization Gradual adjustment to seasonal temp Torphor, Hibernation, Estivation Adaptations to survive extreme climates by conserving energy Torphor Hibernation Sleeplike state Metabolic rate and body temperature drop in response to daily temp (nocturnal animals, hummingbird) State of inactivity over an extended period of time Estivation Seasonal torphor – environment is hot and water is scarce Water Balance Extracellular fluid needs to maintain a constant volume (~15L) of water and balance of solute within the body Mechanism Osmosis Osmosis Water molecules move from a high concentration to a region of lower concentration across a selectively permeable membrane Osmotic pressure Results from a difference in water concentration gradient between the two sides of the selectively permeable membrane Hyperosmotic Hypoosmotic Isoosmotic Hyperosmotic Solution with higher concentration of solute molecules Water tends to move to this side Hypoosmotic Solution with lower concentration of solute molecules Water tends to move from this solution Isoosmotic Solution with the same solute and water concentrations Osmoregulation Process of actively regulating the osmotic pressure of bodily fluids Extracellular fluid = intracellular fluid (isoosmotic) [solute] remains the same [water] remains the same The Excretory System Main functions (with the help of osmoregulation) Concentrate wastes and expel them from the body Regulate fluids and water within the body Organs included Kidney Adrenal gland Ureter Urinary bladder Urethra Removal of Metabolic Waste Waste Origin of Waste Organ of Excretion Ammonia Breakdown of amino acids in the liver kidneys Urea Conversion of ammonia in the liver kidneys, skin Uric Acid Breakdown of purines in food and drink kidneys Carbon Dioxide Cellular respiration (breakdown of glucose) lungs, intestines, skin Bile Pigments Breakdown of porphyrin ring (hemoglobin) intestines Lactic Acid Cellular respiration (breakdown of glucose) kidney Solid Waste Breakdown of food intestine Kidneys Removes waste Balances blood pH Maintain body’s water balance Blood is supplied to kidney via renal artery Re-enters circulatory system via renal vein Nephrons Functional unit of the kidney (1 000 000 per kidney) Regulate water balance Conduct excretion Different sections of the nephron have specialized functions in formation of urine and conservation of water http://www.youtube.com/watch?v=oXcEAH_yesY Urinary Bladder Renal pelvis connects the kidney to the ureter which fills the bladder Holds ~300mL-400mL of urine before exiting the urethra Deamination Occurs in the liver – breakdown of protein Removal of amino group from amino acid Creates ammonia NH₃ (toxic to body) Urea Cycle Ammonia reacts with bicarbonate and 2 ATP molecules to form urea Transported to kidneys where excretion occurs via blood Bicarbonate Buffer System Maintains pH of blood (acid-base homeostasis) Formation of Urine Ultimate goal – conserve water, balance salts, concentrate wastes Urine – hypoosmotic to surrounding body fluids - water tends to move from urine into the body fluids 3 Feature of nephron interact to achieve ultimate goal Arrangement of loop of Henle Difference in permeability Concentration gradient of molecules and ions 3 processes interact to achieve formation of urine Filtration Reabsorption Secretion Formation of Urine: Overall Process Filtration Begins at Bowman’s capsule (selectively permeable membrane) Receives water, ions, glucose, AA and urea from glomerulus Difference of pressure allows for transfer of molecules and ions into capsule 1400L of blood pass through kidneys every day Bowman’s capsule filters ~180L from blood ~1.5L is excreted as urine daily Reabsorption Occurs as fluid from Bowman’s capsule enters proximal convoluted tubule, Loop of Henle and distal convoluted tubule Water, ions and nutrients are transferred back into interstitial fluid and peritubular capillaries via passive and active transport Microvilli inside tubules increase surface area Difference in solute concentration allows water to move across the membrane and back into interstitial fluid via osmosis (aquaporins) Secretion Removal of waste products from the blood and interstitial fluid and secreted into the nephron Include – detoxified poisons, water soluble drugs, metabolites, H⁺ Secretion of H⁺ ions balances acidity in body Reabsorption of HCO₃⁻ occurs simultaneously Buffer system controls pH levels of blood Increased acidity – H⁺ excreted as urine Urine reaches bottom of collecting ducts, flows into renal pelvis, through ureters, into urinary bladder and exits through urethra Kidneys Regulate Blood Oxygen Levels Kidneys monitor blood oxygen levels (RBC’s) If too low – kidneys release erythropoetin (EPO) into the blood stream which stimulates the production of red blood cells Kidney Diseases Renal Failure 2 types Acute – rapid progressive loss of renal function Chronic – slow progressive with long term consequences Injuries, accidents, complications from surgery Diabetes mellitus, uncontrolled hypertension, polycystic kidney diseases Treatments Dialysis Kidney transplant