* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Lecture 3 - IMaGeS Lab
Survey
Document related concepts
Transcript
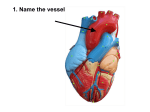
PCB4233: Immunology Dr. Mauricio Rodriguez-Lanetty Email: rodmauri@fiu.edu Phone: 305-3484922 Lecture 3 On January 18th, the lectures will be uploaded to Blackboard Learn On January 21st, a question-based guide covering the first four lectures will be provided Skin Interactions: consequences: Blood vessel Skin Interactions: consequences: Macrophage Blood vessel Skin Interactions: consequences: PRR-PAMP Macrophage Blood vessel Skin Interactions: consequences: PRR-PAMP 1) Phagocytosis of the pathogen Blood vessel 2) Cell signaling that trigger expression of cytokines and chemokines Skin Interactions: consequences: PRR-PAMP A well known example of this! 1) Phagocytosis of the pathogen Blood vessel 2) Cell signaling that trigger expression of cytokines and chemokines Skin Interactions: consequences: PRR-PAMP 1) Phagocytosis of the pathogen Blood vessel CD14 TLR4 2) Cell signaling that trigger expression of cytokines and chemokines Cell membrane Toll-like receptor signaling pathway Skin Interactions: consequences: PRR-PAMP 1) Phagocytosis of the pathogen Bacteria 2) Cell signaling that trigger expression of cytokines and chemokines Blood vessel LPS CD14 TLR4 Cell membrane Skin Interactions: consequences: PRR-PAMP 1) Phagocytosis of the pathogen Bacteria 2) Cell signaling that trigger expression of cytokines and chemokines Blood vessel LPS CD14 TLR4 Cell membrane Activation of transcription factors (NF-kB) Stimulation of gene expression Cytokines (TNF-α, IL-1, CXCL8) Inflammation, migration of leukocytes, adaptive immunity Skin Interactions: consequences: PRR-PAMP 1) Phagocytosis of the pathogen Cytokines Blood vessel 2) Cell signaling that trigger expression of cytokines and chemokines Skin Interactions: consequences: PRR-PAMP 1) Phagocytosis of the pathogen Cytokines Blood vessel Cytokines – blood vessel endothelia cells 2) Cell signaling that trigger expression of cytokines and chemokines Skin Interactions: consequences: PRR-PAMP 1) Phagocytosis of the pathogen Cytokines Blood vessel Cytokines – blood vessel endothelia cells TNF-α 2) Cell signaling that trigger expression of cytokines and chemokines 3) Activate endothelia cells. So more adhesion molecules are expressed, like selectins and ICAMS 4) Vasodilation and increase vascular permeability Skin Interactions: consequences: PRR-PAMP 1) Phagocytosis of the pathogen Chemokines Cytokines Blood vessel Cytokines – blood vessel endothelia cells Chemokines – Leukocytes CXC8 or IL-8 TNF-α 2) Cell signaling that trigger expression of cytokines and chemokines 3) Activate endothelia cells. So more adhesion molecules are expressed, like selectins and ICAMS 4) Vasodilation and increase vascular permeability Skin Interactions: consequences: PRR-PAMP 1) Phagocytosis of the pathogen Chemokines Cytokines Blood vessel Cytokines – blood vessel endothelia cells Chemokines – Leukocytes CXC8 or IL-8 TNF-α 5) Induce chemotaxis 6) Help in the adhesion of phagocyte during migration 2) Cell signaling that trigger expression of cytokines and chemokines 3) Activate endothelia cells. So more adhesion molecules are expressed, like selectins and ICAMS 4) Vasodilation and increase vascular permeability Skin Interactions: consequences: PRR-PAMP 1) Phagocytosis of the pathogen Chemokines Cytokines Blood vessel Cytokines – blood vessel endothelia cells Chemokines – Leukocytes CXC8 or IL-8 TNF-α 2) Cell signaling that trigger expression of cytokines and chemokines 3) Activate endothelia cells. So more adhesion molecules are expressed, like selectins and ICAMS 4) Vasodilation and increase vascular permeability Skin Blood vessel Who are the first to migrate to the site of infection? Skin Neutrophils Blood vessel Do neutrophils look (morphological) similar to macrophages? Skin Neutrophils Blood vessel Skin Neutrophils Blood vessel How they kill the pathogens especially bacteria? Once ingested: inside the phago-lysosome The respiratory burst in macrophages and neutrophils is caused by a transient increase in oxygen consumption during the production of microbicidal oxygen metabolites This occur both in macrophages and neutrophils How important is this Respiratory burst to clear infections? Chronic Granulomatous Disease: a genetic deficiency of NADPH oxidase, so the phagocytes do not produce toxic oxygen species. People with this disease are susceptible to bacterial and fungal infections Skin Neutrophils Blood vessel How they kill the pathogens especially bacteria? Phagocytosis Respiratory burst (a production of a buch nasty reactive oxygen species that kill bacteria) Skin Blood vessel Interferon (another cytokine) induced by viral infection: Interferon induce a state of resistance to viral replication in all cells IFN-α and IFN-β induce the expression of proteins that help to inhibit viral replication Autocrine and paracrine effect Activate dentritic cells and macrophage Skin Neutrophils Blood vessel How they kill the pathogens especially bacteria? Phagocytosis Respiratory burst (a production of a buch nasty reactive oxygen species that kill bacteria) So, do all leukocytes kill through phagocytosis? Skin Blood vessel NK (natural killer) Cells [Non-phagocytic Killer] •Natural killer cells are nonphagocytic and granular lymphocytes that kill abnormal (e.g., infected or malignant) host cells •They account for 5-10% of all lymphocytes in circulation •The lineage of origin is different to macrophages, mast cells and the other granulocytes Skin How they distinguish an infected from a healthy, uninfected cell? Blood vessel NK (natural killer) Cells [Non-phagocytic Killer] •Natural killer cells are nonphagocytic and granular lymphocytes that kill abnormal (e.g., infected or malignant) host cells •They account for 5-10% of all lymphocytes in circulation •The lineage of origin is different to macrophages, mast cells and the other granulocytes