* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download PRENATAL DEVELOPMENT
Vectors in gene therapy wikipedia , lookup
Embryonic stem cell wikipedia , lookup
Cell culture wikipedia , lookup
Cellular differentiation wikipedia , lookup
Cell (biology) wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Somatic cell nuclear transfer wikipedia , lookup
Drosophila melanogaster wikipedia , lookup
Organ-on-a-chip wikipedia , lookup
Cell theory wikipedia , lookup
Cell growth wikipedia , lookup
List of types of proteins wikipedia , lookup
State switching wikipedia , lookup
Chimera (genetics) wikipedia , lookup
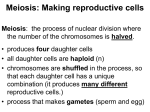
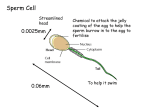
PRENATAL DEVELOPMENT The Female Reproductive System Uterus A muscular chamber about the size and shape of a pear. Located in a woman's abdomen, is a hollow, elastic reproductive organ, where a baby develops during pregnancy. Female anatomy The uterus - is a major female hormoneresponsive reproductive sex organ Within the uterus fetus develops during gestation. The term uterus =womb. One end, the cervix, opens into the vagina; the other is connected on both sides to the Fallopian tubes. Sperm is the male reproductive cell Sperm Chief Characteristics: 1. Tightly packed tip (acrosome) that contains 23 chromosomes that carry genetic information 2. Short neck region 3. Trail to propel it in its search for the ovum 4. Microscopic Fact: Remains capable of fertilizing egg for 24-48 hours after ejaculation Of 200 million sperm that enter the vagina, only about 200 survive the journey to the fallopian tubes, where fertilization occurs Males, at birth, have in their testes those cells that will eventually produce sperm Ovum (Egg) The ovum is the female reproductive cell Chief Characteristics: 1. Round 2. .01 mm in diameter 3. Consistency of stiff jelly 4. Contributes 23 chromosomes Fact: Females already have 1-2 million primal eggs at birth Eggs usually fertilized about 12 hours after discharged from the ovary or they die within 12-24 hours ovulation • When a young woman reaches puberty, she begins to ovulate • a process in which a mature egg cell (also called an ovum), ready for fertilization by a sperm cell, is released from one of the ovaries Her body prepares for a potential pregnancy every cycle, whether or not she want to actually conceive. Under the influence of Follicle Stimulating Hormone (FSH), about 15 to 20 eggs start to mature in each ovary. Although it averages about two weeks, the process to release an egg can take anywhere from about eight days to a month or longer to complete. menstrual cycle Ovulation occurs 14 days before the next menstruation. As the average menstrual cycle lasts 28 days (starting with the first day of one period and ending with the first day of the next menstrual period), most women ovulate on day 14. A menstrual cycle can vary between 21 to 38 days. A woman is generally most fertile (able to become pregnant) a few days before, during, and after ovulation. The corpus luteum remains behind on the interior ovarian wall, and starts releasing progesterone. Progesterone quickly stops the release of all other eggs until the next cycle. The corpus luteum has a finite lifespan, of about 12 to 16 days. Menstruation If the egg does not become fertilized as it travels down the fallopian tube on its way to the uterus, the endometrium (lining of the uterus) is shed and passes through the vagina (the passageway through which fluid passes out of the body during menstrual periods; also called the birth canal), a process called menstruation. Pregnancy If the egg is fertilized by a sperm cell as it travels down the fallopian tube, then pregnancy occurs, it becomes attached to the lining of the uterus In order for conception to occur, though, there must be three factors present: the egg, the sperm a medium in which the sperm can travel to reach the fallopian tubes. Women produce cervical fluid under the influence of increasing levels of estrogen in the first part of the cycle. Sperms can live up to five days in fertile quality cervical fluid 3 Stages in prenatal development: Germinal stage Embryonic stage Fetal stage Principles Cephalocaudal principle Proximodistal principle First Stage: Germinal Starts at conception (fertilization) until implantation 14 days. Conception process When the sperms meets the egg (ovum) in the fallopian tube travel down into the uterus where it implants in the uterine lining and begin to grow (implantation). Conception Conception occurs when the sperm meets and penetrates the ovum, or egg sperm ovum Normally, only one sperms will succeed penetrating through the ovum wall. When one sperms succeeded penetrating the ovum wall, a protective lining will form around it preventing other sperms to enter/penetrate. The combination of ovum & sperms form zygote (with one nucleus). Zygote will later develop into blastosist a complex organism with millions of cells with various functions. Germinal stage (fertilization to 2 weeks) Rapid cell division, increasing complexity and differentiation, and implantation Mitosis Blastocyst Embryonic disk Ectoderm, endoderm, mesoderm Trophoblast Placenta & umbilical cord Amniotic sac & chorion Fertilization: the sperm and egg join in the fallopian tube to form a unique human being. • a fertilized egg, only thirty hours after conception. Zygotic Period (Conception - 1st Week) A zygote is a fertilized egg with 46 chromosomes Genetic potential determined at this time Egg is 2.5 mm in diameter at end of 1st week Mitosis, a process of cell division, occurs during this period Early development of a human embryo Early development of a human embryo Embrio : blastosis burrows into the uterine lining As soon as the fertilized egg burrows into the lining, it starts releasing a pregnancy hormone, HCG (Human Chorionic Gonadotropin) which sends a message back to the corpus luteum left behind on the ovarian wall. HCG signals the corpus luteum to remain alive beyond its usual maximum of 16 days and continuing to release progesterone long enough to sustain the nourishing lining. After several months, the placenta takes over, not only maintaining the endometrium, but providing all the oxygen and nutrients the fetus needs to thrive. Cells Division There are two type of cell division Mitosis and meiosis Reproductive cells divide through meiosis process, while all other body cells divide through the mitosis process Cells Division Mitosis is cell division that results in the duplication of cells; the daughter cells genetic copies of the parent cell. This cell multiplication allows for replacement of old cells, tissue repair, growth and development. Mitosis The creation of new cells through duplication of chromosomes & divisions of cells cells duplicates (From 1 24 16 32, etc) Cells developed into organs, brain, heart etc. Growth & Development You grew from a zygote, or fertilized egg (the fusion of two cells: an egg and a sperm) into an organism with trillions of specialized cells. Mitosis is the process that enabled you to grow and develop after that fateful meeting of ovum and sperm became ‘you’. Cell Replacement Cells must divide in order for an organism to grow and develop, but cell division is also required for maintenance, cell turnover and replacement. Meiosis is Sex Cell (Gamete) Formation In sexually reproducing organisms, some cells are able to divide by another method called meiosis. Meiosis is a complex process by which gametes form; involves duplication and division of reproductive cells and their chromosomes. The number of chromosomes in cells divide into two’s, and each set of cell will receive 1 from each sets of chromosomes makes up 23 sets. This type of cell division results in the production of gametes (eggs or sperm). Meiosis is much more complex than mitosis involves the duplication and subsequent division of chromosomes, meiosis involves two divisions of genetic material. As is the case in mitosis, in meiosis the cell duplicates its chromosome number prior to beginning cellular division. Then nuclear division, the sorting out of the genetic material, begins, and unfolds over the course of 2 cellular divisions that result in 4 gametes. Meiosis is Sex Cell (Gamete) Formation Gametes & Gonads Gametes are haploid (1n) with half the number of chromosomes than the progenitor cell that they arose from. These haploid sex cells arise in specialized reproductive tissue called the gonads. Ovaries (female gonads) and testes (male gonads) are the sites of meiosis. Fertilization & Development Sexual reproduction results in the merging of sperm and egg at fertilization, and brings the chromosome count back to the 2n diploid number necessary for a zygote to have complete genetic information; 2 sets of genetic instructions in 23 pairs of chromosomes. As cells divide, the zygote develops and grows into an embryo, fetus and beyond. These 23 pairs of chromosomes are duplicated with every cell division, and are the genetic material inside nearly every cell of the body. What's the Difference between Mitosis & Meiosis Mitosis is how the cells of our body make more cells for growth, development and repair. Meiosis is how our body makes sex cells, or gametes (eggs or sperm). Mechanisms of Heredity The Genetic Code Basis of heredity is a chemical called deoxyribonucleic acid (DNA), which contains all the inherited material passed from biological parents to children Every cell except the sex cells has 23 pairs of chromosomes--46 in all Genetic action that triggers growth of body and brain is often regulated by hormones Mechanisms of heredity The genetic code DNA and chromosomes Human genome 23 pairs of chromosomes in every cell (46 total) – except sex cells Meiosis – division in sex cells (23 single chromosomes) Mitosis – division in body cells Genetic Code Genetic information are kept in chromosomes ie. A long & complex set of DNA molecules. Genes is a segment of DNA molecules contains instructions for making protein. Human being is said to have 100 trillions of cells in the body with specific functions; and is distributed through 46 chromosomes, ie. 23 from father & 23 from mother. Genetic Foundation Genotype (genetic makeup) Phenotype (observable characteristics) Hereditary composition of the zygote What determines sex? Autosomes – chromosome pairs 1- 22 Sex chromosomes – 23rd pair of chromosomes XX = female Xy = males Determination of a child’s sex What Determines Sex? Sex chromosomes are either X chromosomes or Y chromosomes When an ovum (X) is fertilized by an Xcarrying sperm, the zygote formed is XX, a female When an ovum (X) is fertilized by a Ycarrying sperm, the resulting zygote is XY, a male Choromosomes Boy or girl? Chromosomes determine sex : 23 pairs of sex chromosomes Female : XX pairs of sex chromosomes Male : XY pairs of sex chromosomes FATHER=XY XY (male) MOTHER=XX XX (female) Patterns of Genetic Transmission When an offspring receives two contradictory traits, only one of them, the dominant one shows itself The expression of a recessive trait, occurs only when a person receives the recessive traits from both parents Dominant and recessive inheritance What Causes Multiple Births? Dizygotic (two-egg) twins=fraternal twins Monozygotic (one-egg) twins=identical twins The rise in multiple births is due in part to a trend toward delayed childbearing Infertility Inability to conceive a baby after 12 to 18 months of trying Genetic and Chromosomal Abnormalities Some defects are due to abnormalities in genes or chromosomes, which may result from mutations Many disorders arise when an inherited predisposition interacts with an environmental factor, either before or after birth Sex linked inheritance of a birth defect Genetic Counseling and Testing A chart can show chromosomal abnormalities and can indicate whether a person who appears normal might transmit genetic defects to a child Multiple births Dizygotic and monozygotic twins Increased incidence of multiple births in US Why? Delayed childrearing Fertility drugs Infertility: Alternative ways to parenthood Inability to conceive after 12 to 18 months of trying Multiple causes Too few sperm Too few ova Abnormal ova Disease of the uterine lining Deterioration in quality of ova Blockage of the fallopian tubes Assisted reproduction Artificial insemination Artificial insemination by a donor In vitro fertilization Ovum transfer Surrogate motherhood What are concerns raised by surrogate motherhood? Nature and Nurture Some Characteristics Influenced by Heredity and Environment Adopted children's IQs are consistently closer to the IQs of their biological mothers than to those of their adoptive parents and siblings. Monozygotic twins generally look alike; they are also more concordant than dizygotic twins in their risk for such medical disorders as hypertension (high blood pressure), heart disease, stroke, rheumatoid arthritis, peptic ulcers, and epilepsy Heredity seems to exert a strong influence on general intelligence and also on specific abilities A strong hereditary influence on schizophrenia and autism, among other disorders; found in families 2nd Stage in prenatal development stage Embryonic Stage Embryonic stage (2 to 8 weeks) Rapid growth and development of major body systems and organs A critical period Trimesters Spontaneous abortion (miscarriage) Stillborn Phases in pregnancy: First trimester (week 1-12) 2nd Trimester (week 13 -24) 3rd Trimester (week 25 & above) Proses Persenyawaan Bapa (sperma) ½ sel (23 kromosom X or Y) Ibu (Ovum) ½ sel (23 kromosom X) Persenyawaan zigot Embrio Fetus Baby 2nd Stage: Embryonic Period (2nd Week - 2nd Month) The phase after implantation. after the development of zygote and developing its blastosist. Embryo composed of millions of cells with various functions (week 3-8) 2nd Stage: Embryonic Period (2nd Week - 2nd Month) The differentiation of embryonic cells into layers marks the beginning of the embryo, or embryonic period Period when all body systems form Highly sensitive for susceptibility of congenital malformations, or abnormal conditions with which an infant is born Embryonic Period: End of the 1st Month 1/4 inch (6 mm) long 1 oz. Weight Crescent-shaped with small limb buds on sides Tail with tiny ridges Rudimentary circulatory system is forming Heart begins to beat Growth acceleration Embryonic Period:End of 2nd Month 1.5 inches long Beginning of face, neck, fingers, toes develop Limb buds lengthen Muscles enlarge Sex organs begin to form Rapid brain development Embryo is firmly planted on uterine wall and is receiving nourishment from placenta and umbilical cord 7 weeks Facial features are visible, including a mouth and tongue. The eyes have a retina and lens. The major muscle system is developed, and the unborn child practices moving. The child has its own blood type, distinct from the mother's. These blood cells are produced by the liver now instead of the yolk sac. 3rd stage: Fetal Stage (8 weeks to birth) Embryo develops fetus (baby in the uterus). Cells that represents eyes, head, body, hands, legs further develops larger. The period of consumption until baby is born 40 weeks (sometimes 38-36 weeks). Fetal stage Increased detail of body parts and greatly enlarged body size Finishing touches Fetal behavior Ultrasound Early Fetal Period: 3rd - 6th Month Period of the fetus begins around the 3rd month and continues until delivery Movement first becomes apparent to mother at this time No new anatomical features appear during this period, yet still critical time Early Fetal Period: 3rd Month Rapid growth, 3 inches long at end of 3rd month Sexual differentiation continues Teeth buds emerge Stomach and kidneys begin to function Vocal cords appear Reflex actions felt: opens/closes mouth, clenches fist, sucks thumb Early Fetal Period:4th Month Most rapid growth rate (doubles in length to 68 inches) 6 oz. Weight Hands fully shaped Bony tissue begins to form Early Fetal Period:5th Month Reaches 1/2 of birth length (8-10 inches) Only 10% of birth weight (1/2 lb.) Skin, hair, nails appear Internal organs grow and assume proper anatomical positions Pigmented hair on head & eyebrows appears Early Fetal Period: 6th Month 13 inches long 1 lb. Weight Eyelids reopen and are completed Structurally complete but functionally immature Later Fetal Period: 7th-9th Month/Birth From the 7th month to birth, the fetus triples in weight This is a period of filling out Preparation for birth Later Fetal Period:7th Month A layer of adipose tissue begins to form under skin (serves as both insulator & food supplier) Rapid 2-4 lb. Weight gain 14-16 inches long Fetus is quiet for long periods of time Brain more active and is increasing control over body systems Later Fetal Period:8th Month Fetus is more active (frequent changes in position) Fatty deposits distributed 16-18 inches long 4-6 lbs. Later Fetal Period:9th Month (Birth) 19-21 inches long 6-8 lbs. Birth process is initiated by placenta and contraction of uterine muscles Birth generally occurs after week 40 of gestation (normal is 38-42 wks.) Important parts in the uterus Amniotic Sac Placenta Amniotic fluid Umbilical cord Environmental Influences (Teratogens) Maternal factors Teratogenic – capable of causing birth defects Maternal factors (continued) Prescription and Nonprescription Drugs Medical drugs Thalidomide DES Aspirin Caffeine Cocaine, heroin, or methadone Maternal factors (continued) Tobacco/Nicotine Alcohol Fetal alcohol syndrome Fetal alcohol effects Sexually transmitted diseases and other maternal illnesses Acquired immune deficiency syndrome Radiation Environmental Polution Maternal Diseases Other Maternal factors Exercise & Physical activity Nutrition Emotional Stress Rh Incompartibility Maternal age Paternal factors Environmentally caused defects Cocaine use Age Smoking Monitoring prenatal development Ultrasound Sonogram Sonoembriology Amniocentesis Chorionic villus sampling Embryoscopy Preimplantation genetic diagnosis Umbilical cord sampling (fetal blood sampling) Maternal blood test Prenatal care Why is prenatal care important? How can it be improved? What is the relationship between prenatal care and low birthweight and premature births? How can we tell whether a new baby is healthy and is developing normally? What complications of childbirth can endanger newborn babies, and what can be done to increase the chances of a positive outcome? The birth process Stages of childbirth First stage Second stage Third stage Fourth stage Electronic fetal monitoring Stages of childbirth