* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Chapter 14 - apsubiology.org
Central pattern generator wikipedia , lookup
Neuroregeneration wikipedia , lookup
Caridoid escape reaction wikipedia , lookup
Axon guidance wikipedia , lookup
Development of the nervous system wikipedia , lookup
Feature detection (nervous system) wikipedia , lookup
Optogenetics wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Signal transduction wikipedia , lookup
Premovement neuronal activity wikipedia , lookup
Nervous system network models wikipedia , lookup
End-plate potential wikipedia , lookup
Channelrhodopsin wikipedia , lookup
Pre-Bötzinger complex wikipedia , lookup
Synaptic gating wikipedia , lookup
Haemodynamic response wikipedia , lookup
Neuromuscular junction wikipedia , lookup
Chemical synapse wikipedia , lookup
Synaptogenesis wikipedia , lookup
Endocannabinoid system wikipedia , lookup
Microneurography wikipedia , lookup
Neurotransmitter wikipedia , lookup
Neuroanatomy wikipedia , lookup
Norepinephrine wikipedia , lookup
History of catecholamine research wikipedia , lookup
Stimulus (physiology) wikipedia , lookup
Molecular neuroscience wikipedia , lookup
Circumventricular organs wikipedia , lookup
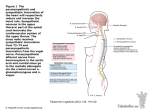
Chapter 14 The Autonomic Nervous System J.F. Thompson, Ph.D. & J.R. Schiller, Ph.D. & G. Pitts, Ph.D. Autonomic Nervous System Overview automatic, involuntary primarily involved in maintaining homeostasis of the internal environment visceral efferent neurons innervate visceral effectors: smooth muscle, cardiac muscle, exocrine glands and endocrine glands The ANS Is Clinically Significant! If you plan to succeed in a HealthRelated Career, you will need to understand the Autonomic Nervous System very well! Two Functional Divisions Parasympathetic and Sympathetic Divisions Structurally, each division consists of nerves, nerve plexuses, and autonomic ganglia Each motor command is carried over a two-cell circuit Most effector organs and tissues receive impulses from both ANS divisions, a dual or parallel innervation The two divisions often serve as antagonists to each other in adjusting and maintaining internal homeostasis Parasympathetic system dominates in sleep and other relaxed or resting states Sympathetic dominates during skeletal muscle activities and various emergency situations (fright, panic, rage, aggression) There is a constant interplay between the two divisions Comparison of Somatic to Autonomic somatic: one motor neuron to skeletal muscle effectors autonomic: two motor neurons to visceral effectors Autonomic Visceral Reflex Arc Two Types of Autonomic Neurons Preganglionic neurons cell bodies in the CNS (brain or spinal cord) transmit Action Potentials from the CNS Postganglionic neurons cell bodies in autonomic ganglia in the periphery transmit APs to effectors Two Cell Motor Pathways in the ANS preganglionic neurons in the sympathetic division, the cell body is located in the lateral gray horns (thoraco-lumbar) of the spinal cord in the parasympathetic division, the cell body is located in various nuclei of brain stem or in the lateral gray horns (cranio-sacral) postganglionic neurons the postganglionic fiber sends impulses to a target organ the effects at the target organ are due to type of neurotransmitter and specific cell surface receptors on the effector cells Dual Innervation The Sympathetic and Parasympathetic Divisions of the ANS innervate many of the same organs Different effects are due to specific molecular differences in the neurotransmitters and in the receptor types on the effectors ANS Dual Innervation The Parasympathetic Division exerts shortlived, highly localized control. The Sympathetic Division exerts long-lasting, diffuse effects. Due to differences in target responsiveness to neurotransmitters Parasympathetic Ganglia parasympathetic terminal ganglia = intramural ganglia ganglia are located very close to or in the wall of the visceral organs each preganglionic neuron synapses with a only few postganglionic neurons parasympathetic preganglionic fibers are long parasympathetic postganglionic fibers are short Sympathetic Ganglia sympathetic trunk = vertebral chain ganglia (paravertebral ganglia) a vertical row on either side of the vertebral column these ganglia are interconnected thoracic and lumbar origin each preganglionic neuron synapses with many postganglionic neurons other sympathetic ganglia are located in the walls of major abdominal arteries short preganglionic fibers long postganglionic fibers ANS Neurotransmitters & Receptors Neurotransmitters Preganglionic - Acetylcholine Postganglionic Parasympathetic - acetylcholine Sympathetic – norepinephrine & in a few locations acetylcholine Receptors Parasympathetic nicotinic - excitatory muscarinic - excitatory or inhibitory Sympathetic alpha - excitatory beta - excitatory or inhibitory ANS Neurotransmitters Acetylcholine (ACh) and norepinephrine (NE) are the two major neurotransmitters of the ANS Cholinergic fibers = ACh-releasing fibers ACh is released by all preganglionic axons and all parasympathetic postganglionic axons Adrenergic fibers = NE-releasing fibers Most sympathetic postganglionic axons Neurotransmitter effects can be excitatory or inhibitory depending upon the receptor type Neurotransmitters and Receptors of the Autonomic Nervous System Receptor Class Nicotinic Muscarinic Agonist Nicotone Muscarine Antagonist Curare Atropine Nicotinic Receptors Nicotinic receptors are found on: Motor end plates (skeletal muscle) All postganglionic neurons of both sympathetic and parasympathetic divisions The hormone-producing cells of the adrenal medulla The effect of ACh binding to nicotinic receptors is always excitatory Muscarinic Receptors Muscarinic receptors occur on all effector cells stimulated by parasympathetic cholinergic fibers and by those few effectors stimulated by sympathetic cholinergic fibers The effect of ACh binding at muscarinic receptors: Can be either inhibitory or excitatory Depends on the receptor type of the target organ Adrenergic Receptors The two fundamental types of adrenergic receptors are alpha and beta Each type has subclasses: (1, 2, 1, 2 , 3) Effects of NE binding to: receptors is generally excitatory to effectors receptors is generally inhibitory to effectors A clinically important exception – NE binding to receptors in the heart is excitatory ANS Neurotransmitters & Receptors See Table 14.3 “Cholinergic and Adrenergic Receptors” (p. 543) for all the details Cholinergic receptors = nicotinic and muscarinic Adrenergic receptors = alpha1,2 and beta1,2,3 These details about receptor subtypes will be very important in later courses, such as Pharmacology (in Nursing) ANS Neurotransmitter Performance Cholinergic fibers/neurons tend to cause relatively short-lived effects due to the rapid hydrolysis of acetylcholine by cholinesterase in the synapse Adrenergic fibers/neurons tend to cause relatively longer-lived effects due to the slower degradation of norepinephrine by catechol-omethyltransferase (COMT) and monoamine oxidase (MAO) in the synapse or in body fluids Adrenergic receptors also respond to the closely-related hormone, epinephrine = adrenalin, secreted by the adrenal medulla Drugs Related to ANS Neurotransmitters Drugs which mimic the action of ACh and NE at their receptors are termed cholinergic and adrenergic agonists respectively Drugs which block or inhibit the action of ACh and NE at their receptors are termed cholinergic and adrenergic antagonists (or “blockers”) respectively Drugs which enhance the action of ACh and NE at their synapses by delaying enzymatic degradation are termed anticholinesterases monoamine oxidase inhibitors (MAO-inhibitors) Drugs Related to ANS Neurotransmitters Table 14-3, p. 537, list examples of a number of autonomic drugs classes and some specific examples. Take a look. You’ll probably recognize some. Many are available in over-the-counter preparations. There are many more. Some of the drug classes will be on the exam But no specific drugs will be on the exam Autonomic Nervous System Review Autonomic Nervous System Online Review Neuroscience For Kids http://faculty.washington.edu/chudler/neurok.html This web site has many good reviews and illustrations. Autonomic Nervous System Controls Different regions of the CNS have responsibility for different functions. The cerebral cortex, limbic system, hypothalamus, and the brain stem cooperate to initiate autonomic motor commands. Autonomic Nervous System Controls Most control is unconscious and originates from the hypothalamus But strong conscious emotional states can trigger autonomic, usually sympathetic, responses Autonomic Nervous System Actions See Table 14.4 (pg. 538) for complete details for the responses of each effector organ Parasympathetic S(alivation) L(acrimation) U(rination) D(efecation) metabolic “business as usual” “rest and digest” – “feed and breed” – basic survival functions Sympathetic fight or flight = emergency “survival” situations any increase in skeletal muscular activity for these activities - increase heart rate, blood flow, breathing decrease non-survival activities - food digestion, etc. Parasympathetic Tone Parasympathetic tone: Slows the heart Directs normal activities of the digestive and urinary systems The sympathetic division can override these effects during times of stress or muscular exertion Drugs that block parasympathetic stimuli increase heart rate and interfere with fecal and urinary retention Cooperative Effects ANS cooperation is involved in the complex control of the cardiovascular system ANS cooperation is also seen in control of the external genitalia during sexual activities Parasympathetic fibers cause vasodilation and are responsible for erection of the penis and clitoris Sympathetic fibers cause ejaculation of semen in males and reflex peristalsis in the female reproductive tract Sympathetic Stimulation Sympathetic stimulation is long-lasting because norepinephrine (NE): NE is inactivated more slowly by MAO and COMT NE is an indirectly acting neurotransmitter, triggering a second-messenger system NE and epinephrine are released into the blood by the adrenal medulla in certain situations and remain there until inactivated by liver enzymes Solitary Sympathetic Stimulation Regulates some effectors not innervated by the parasympathetic division Therefore, acting more as an on-off switch These include the adrenal medulla, sweat glands, arrector pili muscles, kidneys, and most blood vessels Solitary Sympathetic Stimulation The sympathetic division controls: Thermoregulatory responses to heat Cutaneous vasodilation and sweating Release of renin from the kidneys Increased blood pressure from a complex regulatory response Metabolic effects (in a complex coordination with the endocrine system) increases the metabolic rate of body cells elevates blood glucose levels for use by nervous tissue shifts cellular metabolism to fats for other tissues stimulates the reticular activating system (RAS) of the brain, increasing mental alertness These actions serve to support the body during strenuous physical activities and emergencies but may contribute to undesirable side effects in cases of long term stress such as illnesses Sympathetic Tone The sympathetic division controls blood pressure, keeping the blood vessels in a continual state of partial constriction (vasomotor tone) Blood pressure rises or falls with sympathetic activity Blood is also diverted to or away from different organ systems depending on the level of muscular activity or the presence of emergency or stressful states Alpha-blocker drugs inhibit vasomotor tone and are used to treat hypertension Autonomic Nervous System Actions Structure Sympathetic Stimulation Parasympathetic Stimulation iris of the eye pupil dilation pupil constriction salivary glands reduce salivation increase salivation oral/nasal mucosa reduce mucus production increase rate and force of contraction increase mucus production decrease rate and force of contraction relax bronchial smooth muscle constrict bronchial smooth muscle heart lung Autonomic Nervous System Actions Structure Sympathetic Stimulation Parasympathetic Stimulation stomach reduce peristalsis; decrease gastric secretions increase peristalsis; increase gastric secretions small intestine reduce peristalsis; decrease intestinal secretions increase peristalsis; increase intestinal secretions large intestine reduce peristalsis; decrease intestinal secretions increase peristalsis; increase intestinal secretions liver increase conversion of glycogen to glucose; release glucose into bloodstream n/a Autonomic Nervous System Actions Structure Sympathetic Stimulation Parasympathetic Stimulation kidney decrease urinary output increase urinary output urinary bladder wall relaxed; sphincter closed wall contracted; sphincter relaxed adrenal medulla secrete epinephrine and norepinephrine n/a sweat glands increase sweat secretion n/a blood vessels increase supply to skeletal decrease supply to skeletal muscles; decrease supply to muscles; increase supply to most viscera most viscera Developmental Aspects of the ANS During youth, ANS impairments are usually due to injury In old age, ANS efficiency decreases, resulting in constipation, dry eyes, and orthostatic hypotension Orthostatic hypotension is a form of low blood pressure that occurs when sympathetic vasoconstriction centers respond slowly to positional changes Raynaud’s Disease causes sudden severe vasoconstriction in the fingers, toes and, occasionally, the ears and nose during a Raynaud’s attack, or episode, several skin color changes (pallor, cyanosis, rubor) may occur, which are often accompanied by paresthsias, a throbbing or burning sensation, cold, or numbness ischemia can be so extreme as to cause gangrene The exact cause of Raynaud’s Disease remains unknown. Referred Pain Visceral afferents run in the same nerves with somatic afferents Pain in the viscera is transferred or interpreted as if it came from somatic areas Heart attack afferents in T1 - T5 pain in the chest, arm, neck or face Risk Factors For Hypertension age heredity race gender weight diet lifestyle/activity level stress: overstimulates sympathetic division? alcohol tobacco End Chapter 14 Some additional information is presented in slides beyond this end point for the lecture. While you will not be tested on this additional material in 2010, you will see it again in some professional courses! Structure of the Autonomic Nervous System Preganglionic neuron somata in the thoracic and lumbar spinal cord segments. Preganglionic neuron somata in the brain and sacral spinal cord. Preganglionic neurons synapse onto postganglionic neurons in the sympathetic chain ganglia. Preganglionic neurons synapse onto postganglionic neuron ganglia near or in the target organs. The postganglionic neurons extend a long distance (usually) to the target organs. The postganglionic neurons do not extend a long distance to the target organs. Parasympathetic and Sympathetic Divisions Structurally, each division consists of nerves, nerve plexuses, and autonomic ganglia Each motor command is carried in a two-cell circuit Most effector organs and tissues receive impulses from both divisions, a dual or parallel innervation The two divisions often serve as antagonists to each other in adjusting and maintaining internal homeostasis Parasympathetic system dominates in sleep and relaxation Sympathetic dominates during vigorous activity/strong emotion sympathetic parasympathetic preganglionic fiber short, myelinated, cholinergic long, myelinated, cholinergic postganglionic fiber long, unmyelinated, usually adrenergic sympathetic chain (= paravertebral), collateral (= prevertebral), adrenal medullae fight or flight, “E” situations short, unmyelinated, cholinergic ganglia dominant? terminal (on or in effector) (= intramural) rest and relaxation, “SLUD” Parasympathetic Pathways Cranial Outflow vial cranial nerves III, VII, IX, and X Cranial nerves III, VII, & IX innervate structures in head Cranial Nerve X (Vagus) innervates ventral body cavity; carries 90% of parasympathetic fibers Sacral Outflow Innervates distal half of large intestine, urinary bladder, ureters, & genitalia Sympathetic Ganglia sympathetic trunk ( = sympathetic chain or paravertebral) ganglia lateral to vertebrae collateral (=prevertebral) ganglia are located near the major abdominal arteries adrenal medullae function as sympathetic ganglia, but neurotransmitters released into blood Sympathetic Paths Sympathetic Paths All preganglionic fibers exit spinal cord via ventral root of spinal nerve, travel into ventral ramus, and into sympathetic chain ganglion via white ramus communicans Then, 1 of 4 (sometimes overlapping) possibilities: 1. synapse with postganglionic neurons at that level of sympathetic chain 2. travel up and/or down sympathetic chain to synapse with postganglionic neurons at other level(s) 3. Pass through sympathetic chain to prevertebral ganglion (via splanchnic nerves) and synapse with postganglionic neurons there 4. (pass through prevertebral ganglion to adrenal medullae) Unique Roles of the Sympathetic Division Regulates many functions not subject to parasympathetic influence These include the activity of the adrenal medulla, sweat glands, arrector pili muscles, kidneys, and most blood vessels The sympathetic division controls: Thermoregulatory responses to heat Release of renin from the kidneys Metabolic effects: increased metabolic rate, increased blood glucose, fat breakdown (lipolysis) Interactions of ANS Divisions Antagonistic: most common, organs stimulated by one division inhibited by the other Sympathetic and Parasympathetic Tone Sympathetic tone controls most blood vessels (even at rest) Parasympathetic tone controls the normal activity of the heart, digestive, and urinary systems Cooperative Effects Important in normal sexual function Thermoregulatory Responses to Heat Applying heat to the skin causes reflex dilation of blood vessels Systemic body temperature elevation results in widespread dilation of blood vessels This dilation brings warm blood to the surface and activates sweat glands to cool the body When temperature falls, blood vessels constrict and blood is retained in deeper vital organs Release of Renin from the Kidneys Sympathetic impulses activate the kidneys to release renin Renin is an enzyme that promotes increased blood pressure Metabolic Effects The sympathetic division promotes metabolic effects that are not reversed by the parasympathetic division Increases the metabolic rate of body cells Raises blood glucose levels Mobilizes fat as a food source Stimulates the reticular activating system (RAS) of the brain, increasing mental alertness Localized Versus Diffuse Effects The parasympathetic division exerts shortlived, highly localized control The sympathetic division exerts long-lasting, diffuse effects because NE: 1. Is inactivated more slowly than Ach 2. Acts indirectly, using a second-messenger system 3. And epinephrine are released into the blood and remain there until destroyed by the liver Localized Versus Diffuse Effects The parasympathetic division exerts localized control because preganglionic fiber travels directly to specific targets and synapses with fewer ganglionic neurons acetylcholine is rapidly degraded The sympathetic division exerts diffuse effects because preganglionic fibers branch and synapse with many ganglionic neurons stimulation of adrenal medullae causes secretion of epinephrine into blood slower inactivation of norepinephrine and epinephrine Effects of Drugs (see Table 14.4, p. 545) Atropine – blocks parasympathetic effects Neostigmine – inhibits acetylcholinesterase and is used to treat myasthenia gravis Tricyclic antidepressants – prolong the activity of NE on postsynaptic membranes Over-the-counter drugs for colds, allergies, and nasal congestion – stimulate -adrenergic receptors Beta-blockers – attach mainly to 1 receptors and reduce heart rate and prevent arrhythmias Drugs Which Influence the ANS Table 14.4.1 Drugs that Influence the ANS Drugs that Influence the ANS Drugs Which Influence the ANS Table 14.4.2 End Additional Material on Chapter 14