* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Respiratory System - eCurriculum
Survey
Document related concepts
Transcript
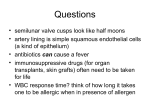
Respiratory System Dr. Jack L. Haar Functions of Respiratory System Transport air to and from lungs Maintains airway patency Regulates air temperature Humidifies air Decreases air velocity Cleanses air Gaseous exchange Olfaction Phonation MAJOR SUBDIVISIONS – Extrapulmonary portion – Intrapulmonary portion Extrapulmonary portion 1. Nasal cavity Nasal 2. Pharynx Oral Laryngeal 3. Larynx 4. Trachea 5. Primary bronchi Extrapulmonary portion 1. Nasal cavity Nasal 2. Pharynx Oral Laryngeal 3. Larynx 4. Trachea 5. Primary bronchi MAJOR SUBDIVISIONS – Extrapulmonary portion – Intrapulmonary portion Intrapulmonary portion Secondary bronchi Larynx Trachea 1. Secondary bronchi 2. Bronchioles (and terminal bronchioles) 3. Respiratory bronchioles 4. Alveolar ducts 5. Alveoli Intrapulmonary portion 1. Secondary bronchi 2. Bronchioles (and terminal bronchioles) 3. Respiratory bronchioles 4. Alveolar ducts 5. Alveoli Classification by function: Conducting portion 1. Nasal cavity 2. Pharynx 3. Larynx 4. Trachea 5. Primary bronchi 6. Secondary bronchi 7. Bronchioles (and terminal bronchioles) Classification by function: Respiratory portion 1. Respiratory bronchioles 2. Alveolar ducts 3. Alveolar sacs 4. Alveoli Terminal bronchiole RB AS RB AD Alveoli Histology overview of respiratory passageways Mucosa: epithelium, lamina propria and muscularis mucosa Epithelium: pseudostratified columnar epithelium with cilia and goblet cells = Respiratory epithelium Layers of “typical” conducting passageway Lamina propria Vascularized Longitudial arranged elastic fibers Deepest layer Elastic lamina OR Muscularis mucosae OR Neither Submucosa – connective tissue layer; contains mixed (mucous and serous secreting glands in larger passageways) Bone or Cartilage – present to level of bronchioles where it drops out Adventitia - connective tissue TRANSITIONS – Layers become thinner and drop out – Epithelium - decreases in height - goblet cells drop out - cilia disappear – Mixed glands drop out – Cartilage drops out Wall of alveolus where gas exchange occurs Alveolus (Inter)alveolar Septum Simple squamous epithelium Connective tissue core Reticular + elastic fibers and CT cells Capillaries Alveolus Cap Simple squamous epithelium Variation on this layering theme MAJOR SUBDIVISIONS – Conducting portion Conducts air from exterior to where – Respiratory portion gas can be exchanged, i.e., alveoli Extrapulmonary of Conducting Portion Nasal cavities Non-olfactory region Vestibules – transition from skin Non-olfactory region to respiratory epithelium Nasal fossae Respiratory epithelium, Abundant blood vessels Muscularis mucosae absent Bones and cartilage for patiency Nasal cavity Non-olfactory region Resp. epith. Lam. propria NO musc. muc. Submucosa (some cartilage) Bone Nasal cavity Olfactory region Olfactory region U-shaped area in posterior, superior regions of nasal fossae Superior concha Non-olfactory region Olfactory region Nasal cavity “Typical” nasal mucosa Olfactory mucosa Olfactory cells: bipolar neurons, single dendrite extends to surface terminates in olfactory vesicle, non-motile cilia extend over surface Supporting cells and basal cells as reserve Olfactory “Typical” nasal mucosa epithelium Olfactory mucosa Nasal cavity Muscularis mucosae not present Lamina propria blends with submucosa Bowmans glands flush odorants Serous glands of Bowman “Typical” nasal mucosa Olfactory mucosa Pharynx Nasal Oral Laryngeal Extrapulmonary Components of Conducting Portion 1. Nasal cavity 2. Pharynx 3. Larynx 4. Trachea 5. Primary bronchi 6. Secondary bronchi 7. Bronchioles and terminal bronchioles Extrapulmonary-Conducting Larynx Larynx Extrapulmonary-Conducting 1. 2. 3. 4. 5. 6. 7. 8. Epiglottal cartilage Thyroid cartilage Cricoid cartilage Tracheal cartilages Vestibule False vocal fold Ventricle True vocal fold with vocal ligament (dense reg elastic CT) 9. Vocalis muscle 1 5 6 7 2 8 9 3 3 4 2 Trachea Extrapulmonary-Conducting Larynx MOST of mucosa is a “typical” respiratory mucosa with NO musc. mucosae. EXCEPTIONS: Stratified squamous moist epithelium covering epiglottis and true vocal fold False vocal fold VL VM Mixed glands in submucosa Cartilage for patency Thyroid and cricoid are hyaline Epiglottis and smaller cartilages are elastic Vocal apparatus False vocal folds Ventricle True vocal folds Vocal ligament - dense regular elastic CT Vocalis muscle – skeletal muscle Extrapulmonary of Conducting Portion 1. Nasal cavity 2. Pharynx 3. Larynx 4. Trachea 5. Primary bronchi 6. Secondary bronchi 7. Bronchioles and terminal bronchioles Trachea and Primary Bronchi are identical Mucosa Respiratory epithelium with prominent basement membrane Longitudinal section Esophagus Trachea LUMEN Elastic lamina of longitudinally arranged elastic fibers Mixed glands in submucosa Cartilage rings for patency Intrapulmonary Components of Conducting Portion 1. Nasal cavity 2. Pharynx 3. Larynx 4. Trachea 5. Primary bronchi 6. Secondary bronchi 7. Bronchioles and terminal bronchioles Secondary bronchus B 2nd Bronchus Pulm BV Pulm BV Bronchiole B Surrounded by ALVEOLI 2nd Bronchus Secondary bronchus Surrounded by ALVEOLI Mucosa Resp epithelium Lamina propria Musc. mucosae Submucosa Mixed glands Cartilage plates Adventitia Cartilage Intrapulmonary of Conducting Portion 1. Nasal cavity 2. Pharynx 3. Larynx 4. Trachea 5. Primary bronchi 6. Secondary bronchi 7. Bronchioles and terminal bronchioles Walls of Bronchi and Bronchioles continue to decrease in size Transition from secondary bronchus to bronchiole Bronchus Bronchiole Bronchioles No mixed glands No cartilage Epithelium: respiratory in largest bronchioles Epithelium: simple columnar with cilia in terminal bronchioles Terminal bronchiole Clara cells present among simple columnar epithelial cells Dome-shaped Non-ciliated with granules Secretions lower surface tension Clara cells Lamina propria: longitudinally arranged elastic fibers Muscularis mucosae: smooth muscle at greatest thickness Submucosa: no glands, no cartilage, no bone Elastic fibers Smooth muscle MAJOR SUBDIVISIONS – Conducting portion – Respiratory portion Where gas exchange actually occurs, i.e., alveoli Transitions Bronchiole to Terminal bronchiole to Respiratory bronchiole B TB RB Transitions of bronchioles Conducting portion Respiratory portion Respiratory bronchiole Continues to decrease in diameter and thickness Respiratory bronchiole Simple cuboidal epithelium Elastic fibers in lamina prop. Muscularis mucosa of smooth muscle Alveoli bulge off of wall Alveolar duct RB Alveoli increase in number Wall is reduced to rings A A A AD Alveolar duct Alveoli increase in number Wall is reduced to rings Alveolar sac Multiple alveoli No wall of cuboidal cells Alveoli Thin walled chambers, 200μm diameter, for gas exchange Interalveolar septum separates alveoli Interalveolar septum CT core Elastic/reticular fibers Fibroblasts Macrophages Capillaries which form 80% of alveolar surface Interalveolar septum CT core Elastic/reticular fibers Fibroblasts Macrophages Capillaries which form 80% of alveolar surface Epithelium lining alveoli Pulmonary epithelial cells (Small alveolar or type I) Lines 95% of alveolar surface Epithelium lining alveoli Pulmonary epithelial cells (Small alveolar or type I) Lines 95% of alveolar surface Epithelium lining alveoli Septal cells (Great alveolar or type II) Regenerate type I and type II cells Epithelium lining alveoli Septal cells (Great alveolar or type II) Regenerate type I and type II cells Mitochondria, RER, Golgi Vacuoles containing the phospholipid surfactant Surfactant lowers surface tension of alveoli Epithelium lining alveoli Surfactant Extracellular fluid layer lining alveoli Lowers surface tension, preventing collapse of alveoli during expiration Covers underlying aqueous hypophase Appears during last weeks of gestation Respiratory distress syndrome or hyaline membrane disease may result Macrophages May be found in the CT core of interalveolar septum Alveolar macrophages are in the alveolar space Kohn’s pores Opening in interalveolar septa Equalize pressure between alveoli Facilitate transfer of bacteria between alveoli Air - blood barrier Pulmonary epithelial cell and its basal lamina Capillary endothelial cell and its basal lamina Air - blood barrier Pulmonary epithelial cell and its basal lamina Capillary endothelial cell and its basal lamina Air - blood barrier Pulmonary epithelial cell and its basal lamina Capillary endothelial cell and its basal lamina Pleura Mesothelium with C.T. Visceral layer Parietal layer Function Lubrication Pleura Alveolus Vascular supply to lungs Blood to and from alveoli Pulmonary artery Adjacent to bronchial tree Vascular supply to lungs Blood to and from alveoli Pulmonary artery Adjacent to bronchial tree Carries unoxygenated blood Vascular supply to lungs Blood to and from alveoli Capillary plexus in interalveolar septa Pulmonary veins Travel away from bronchial tree Carry oxygenated blood Nutrient vessels Bronchial arteries Vessels within wall of bronchial tree Supply nutrients to passageways themselves Nutrient vessels Bronchial arteries Vessels within wall of bronchial tree Supply nutrients to passageways themselves Pathology Effects of smoking Running the numbers web site http://www.portfolio.com/interactivefeatures/2007/12/running-the-numbers Pathology Nasal sinues Emphysema Asthma Chronic bronchitis Pneumonia Functions of Respiratory System Transport air to and from lungs Maintains airway patency Regulates air temperature Humidifies air Decreases air velocity Cleanses air Gaseous exchange Olfaction Phonation TB or not TB? That is the congestion. Consumption be done about it? Of cough, Of cough, But it will take a lung, lung time! -Walter Shakespear http://www.path.uiowa.edu/virtualslidebox/ Table of Contents Lung and respiratory tract Lung (3 slides) http://java.vcu.edu/som-histology/ Respiratory Lung Trachea I Trachea II