* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The uvea - TOP Recommended Websites
Gastroenteritis wikipedia , lookup
Infection control wikipedia , lookup
Inflammation wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Germ theory of disease wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Chagas disease wikipedia , lookup
Neuromyelitis optica wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Sarcoidosis wikipedia , lookup
Acute pancreatitis wikipedia , lookup
Sarcocystis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Globalization and disease wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Kawasaki disease wikipedia , lookup
Rheumatoid arthritis wikipedia , lookup
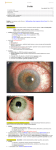
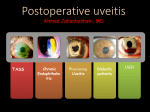
THE UVEA Švehlíková G. Department of Ophthalmology LF UPJS v Košiciach Prednosta: prof. MUDr. Juhás T., DrSc THE UVEA - A. iris B. ciliary body C. choroid CONGENITAL ANOMALIES Heterochromia Iris bicolor Coloboma Mezodermal dysgenesis Aniridia Cysts Iris cyst Heterochromia Iris bicolor Iris coloboma Retinochoroidal coloboma Aniridia Iridocorneal dysgenesis a group of very rare, congenital, usually bilateral conditions resulting from abnormal embryological development of the anterior segment Axenfeld-Reiger syndrome congenital malformations of the face, teeth, and skeletal system Peter's anomaly systemic abnormalities include craniofacial dysostosis, hydrocephalus, pulmonary hypoplasia, cleft lip and palate, cardiac, and GU malformations UVEITIS CLASSIFICATION - Anatomical Anterior Intermediate Posterior Panuveitis UVEITIS Anterior – iritis, iridocyclitis Intermediate – pars planitis, vitritis Posterior – choroiditis, retinitis, vasculitis CLASSIFICATION - CAUSES Infectious Non-infectious causes immunological Idiopatic Masquerade sy INFECTIOUS UVEITIS parasitic uveitis toxoplasma retinitis, toxocariasis, onchocerciasis, cysticercosis viral uveitis – CMV, HSV, HZV fungal uveitis – histoplasmosis, candida bacterial uveitis – TBC, syphilis, borreliosis, leprosy CLASSIFICATION - acute – sudden, less than 3 month chronic - may be asymptomatic, longer than 3 month granulomatous non-granulomatous ACUTE ANTERIOR UVEITIS (AAU) symptoms: pain, photosensitivity to light redness with no mucopurulent discharge mild blurring of vision may be noted most cases of AAU are unilateral ACUTE ANTERIOR UVEITIS CLINICAL SIGNS Intraocular pressure (IOP) - is often lower in the eye with iritis secondary to a decrease in aqueous production by the inflamed ciliary body - in some cases, the IOP may be elevated as a result of altered aqueous outflow; this may be more common in viral anterior uveitis ACUTE ANTERIOR UVEITIS CLINICAL SIGNS Conjunctiva: - typically perilimbal injection termed ciliary flush - less commonly, generalized redness of the bulbar conjunctiva - not found in Fuchs heterochromic iridocyclitis or the anterior uveitis associated with juvenile idiopathic arthritis ACUTE ANTERIOR UVEITIS CLINICAL SIGNS Cornea Keratic precipitates (KPs) may be present - clusters of lymphocytes, polymorphs on the endothelium - in nongranulomatous iritis, they tend to be small - in granulomatous medium and large size called "mutton fat" ACUTE ANTERIOR UVEITIS CLINICAL SIGNS Anterior chamber: Flare, cells, and/or hypopyon may be present hypopyon AQUEUS HUMOR Cells – inidicate disease activity cells degree 0-5 0 6-15 1 16-25 2 26-50 3 > 50 4 Flare - protein in the aqueous due to breakdown of the bloodaqueous barrier flare degree none 0 faint 1 moderate (iris and lens detail clear) 2 marked (iris and lens detail hazy) 3 intense (fibrin or plastic aqueous ) 4 ACUTE ANTERIOR UVEITIS CLINICAL SIGNS Iris posterior synechiae may be present inflammatory nodules are usually present in granulomatous iritis sector atrophy heterochromia and loss of iris stromal detail are suggestive of Fuchs heterochromic iridocyclitis CHRONIC ANTERIOR UVEITIS presents as recurrent episodes, with minimal acute symptoms may be granulomatous or non- granulomatous less common symptoms: many patiens – asymptomatic until development of complications CHRONIC ANTERIOR UVEITIS CLINICAL SIGNS Conjunctiva – eye – usualy white Aqueous cell – vary Aqueous flare – severity may act as an indicator of activity Keratic precipitates Iris nodules – typically in granulomatous uveitis - Koeppe, Busacca nodules INTERMEDIATE UVEITIS - chronic, relapsing disease vitreus is the major site of the inflamation idiopatic or assocciated with a systemic disease: Multiple sclerosis Sarcoidosis Lyme disease INTERMEDIATE UVEITIS CLINICAL SIGNS - Symptoms: blurred vision, usualy unilateral, but condition is usualy bilateral often asymetrical Signs: Anterior uveitis – mild or severe Vitreous – cells, condensation, ´snowballs´ Posterior segment – peripheral periphlebitis, ´snowbanking´ – greywhite fibrovascular plaque POSTERIOR UVEITIS Symptoms : vary – location of the inflammatory focus - patient with peripheral lesion – floaters - patient with a lesion in macula – impaired central vision POSTERIOR UVEITIS CLINICAL SIGNS Retinitis – focal or multifocal, active lesions – whitish retinal opacities with indistinct borders, as the lesions resolves, the borders become better defined Choroiditis – focal, multifocal, geographic, active –yellow nodule Vasculitis – primary or secondary to retinitis DIAGNOSTIC EXAMINATION METHODS - - Laboratory testing Blood count, differential blood count, liver enzymes, kidney function parameters ( urea, creatinin ) Antibody tests – serology – syphilis, borellia, toxoplasmosis, toxocara, HSV, HZV, HIV, Autoantibodies – ANA, ANCA, anticardiolipin antibodies, rheumatoid factor HLA testing FA, OCT Radiological investigation ( chest X-ray, X-ray of the sacroiliac joint) Skin test – tuberculin test Histopathology – biopsy – skin, conjunctiva, lacrimal gland, aqueous samples for PCR, vitreous biopsy Other – USG abdomen, MRI – SM,.. TH Immune-mediated uveitis – antiinflamatory and immunosupresive agents Infectious diseases - ATB MYDRIATICS - - Indications: relieve spasm of the ciliary muscle and pupillary sphincter breakdown formed PS Short-acting : - Tropicamide - 6 hours - Cyclopentolate - 24 hours - Phenylephrine - 3 hours, no cycloplegic effect Long-acting : - Homatropine - 2 days - Atropine - 2 weeks TOPICAL STEROIDS only anterior uveitis frequency depends of severity of inflammation AAU – 5-6 weeks CAU – months – years weak steroid preparations Complications – cataract, elevation of IOP PERIOCULAR STEROIDS Advantages - therapeutic concentration behind the lens - prolonged effect Indication - unilateral intermediate or posterior uveitis, CME - Bilateral posterior uveitis systemic steroids contraindicated - Poor compliance with systemic or topical medication Complication: - Elevation IOP, ptosis, extraocular muscle paresis, ON injury, ... SYSTEMIC STEROIDS - - - oral prednisone or i.v. methylprednisolone 1g/day 2-3 days Indications : intermediate uveitis unresponsive to sub-Tenon inj. posterior uveitis or panuveitis particulary bilateral rarely anterior uveitis resistant to topical th - - Contraindications poorly controlled DM peptic ulceration osteoporosis active systemic infection psychosis Rules to administration: start with large dose Prednison 1-2 mg/kg/day – given in single morning dose maintained until clinical effect is seen reduce slow ANTIMETABOLITES Azathioprine – longterm effect, chronic Indications diseases - sight-threatering uveitis – Methotrexate – bilat., reversible, nonuveitis associated infectius, not respond to with sarcoidosis and steroid th JIA - Patients with intolerable Mycophenolate side-effect from systemic mofetil steroids Treatment should continue 6-24 months IMMUNE MODULATORS Cyclosporin Indications - drug of choice for Behcet sy, intermediate uveitis, sympathetic ophthalmitis, idiopathic retinal vasculitis Side-effect: nephrotoxicity, hyperlipidaemia, hepatotoxicity, hypertension Tacrolimus Indications - an alterantive to cyclosporine BIOLOGICAL BLOCKERS - may be useful - IL2 receptor antagonists - Anti-tumor necrotic factor (TNF) alpha therapy Infliximab ( Remicade ) Adalimumab (Humira ) fully human monoclonal antibody against TNFalpha subcutaneous administration - Patients with retinal vasculitis, Behcet sy when resistent to conventional th initially developed to treat systemic inflammatory diseases or to prevent organ transplant rejection, but have been used off-label to treat uveitis or ocular inflammation ANTERIOR NON-GRANULOMATOUS UVEITIS Non-infectious causes Infectious causes – leptospirosis, rickettsioses,.. Idiopatic uveitis ANTERIOR NON-GRANULOMATOUS UVEITIS NON-INFECTIOUS CAUSES 1. 2. 3. 4. 5. 6. 7. HLA B 27 acute anterior uveitis Juvenile idiopathic artritis Bechcet disease Tubulointerstitial nephritis and uveitis sy Kawasaki disease Lens-induced uveitis Traumatic uveitis 1. HLA B 27 ACUTE ANTERIOR UVEITIS - typically unilateral, severe, recurent - Isolated Associated with systemic disease: *ankylosing spondylitis - M. Bechterev – inflamation, calcification and ossification of ligaments of the axial skeleton *Reiters sy – uretritis, arthritis, uveitis *psoriatic arthritis * ulcerative colitis, Crohn´s disease 2. JUVENILE IDIOPATHIC ARTRITIS Inflammatory arthritis of at least 6 weeks duration, occuring before the age of 16 y Uveitis: -presentationasymptomatic Signs- uninjected eye even in presence of severe uveitis - small precipitates - hypopyon – absent - PS – common No correlation between the activity of joint and eye inflammation 3. BEHCET DISEASE Idiopathic, systemic disease characterized by recurent episodes of orogenital ulceration and obliterative vasculitis young males, Japanese and eastern Mediterranean, HLA-B5 associated Oral, genital ulceration Skin- erythema nodosum, pustules, ulceration, cutaneous hypersensitivity Arthritis- non-destructive, wrists and ankles Ocular complication : reccurent AAU – may be bilat., mild, retinal vasculitis, vitritis FUCH´S UVEITIS FUCHS HETEROCHROMIC IRIDOCYCLITIS first described by Fuchs in 1906 chronic, unilateral signs - precipitates are small, stellate, grey-white, - small nodules at the pupillary border - absence of PS - vitritis - aqueous humor – mild flare and cellular reaction - iris atrophy, heterochromia Complications – cataract, glaucoma TH- topical steroids uneffective, mydriatics unnecessary – noPS POSNER-SCHLOSSMAN SYNDROME recurrent attacks of unilateral, acute mild anterior uveitis with raised IOP rare, young adults IOT ↑ few hours to several days intervals between attack vary Presentation – mild discomfort, haloes Signs – corneal epithelial edema, few aqueous cells, fine precipitates, gonioscopy – open angle Th – topical steroids, antiglaucomatics GRANULOMATOUS UVEITIS Acute granulomatous Herpes simplex/zoster syphilis lens-induced Chronic, granulomatous syphilis tuberculosis leprosy VKH sympathetic ophthalmia sarcoidosis GRANULOMATOUS UVEITIS Infectious granulomatous Herpes simpex/zoster Syphilis Tuberculosis Leprosy Boreliosis Toxoplasmosis Toxacariasis Fungal uveitis Non infectious granulomatous VKH Sympathetic ophthalmia Sarcoidosis SM VOGT- KOYANAGI- HARADA DISEASE VKH multisystem autoimmune disorder against the melanocytes depigmentation after acute inflammation in the skin ( alopecia, poliosis ) and uvea ocular involvement – bilateral uveitis SARCOIDOSIS chronic multisystem granulomatous disease of unknown etiology noncaseating granulomas predominantly affects lungs and intrathoracic lymph nodes, but any organ can by involved involvement of the eyes and adnexa occurs in 25-80% Ocular manifestation of sarcoidosis Adnexal involvement: Orbital lacrimal gland granuloma Extraocular muscles granuloma Lid granuloma Conjunctiva granuloma Conjunctivitis Episcleritis, scleritis Keratitis Uveitis granulomatous or nongranulomatous Anterior veitis Intermediate uveitis Posterior uveitis Panuveitis Optic nerve involvement Papilitis Optic disc granuloma Papilledema SYMPATHETIC OPHTHALMIA bilateral, panuveitis, that occurs after trauma or surgery eye responsible for initiation – exiting fellow eye – sympatizing eye prevalence 0,06-0,01% pathogenesis – aberrant immune response to ocular self-antigens in predisposed individuals HERPETIC VIRAL UVEITIS DNA viruses latent, recurring infections HSV, HZV,CMV Intraocular infection: - Anterior uveitis - Posterior uveitis HERPES SIMPEX/ZOSTER ACUTE RETINAL NECROSIS ARN Unilateral or bilateral – TH: acyclovir, ganciclovir, healthy patients characterized by anterior uveitis, vitritis, and retinal vasculitis with confluent areas of retinal necrosis initially affects the peripheral retina and then extends In contrast, progressive outer retinal necrosis (PORN) syndrome is seen in immunocompromised patients with a uveal inflammation and vasculitis, which spreads rapidly throughout the fundus PORN usually shows rapid progression - very poor prognosis Antiviral treatment should be given CMV RETINITIS primary CMV infection universally leads to a latent state in many cells, which serve as reservoirs for transmission and reactivation during periods of immunodeficiency reactivation of latent CMV in immunosuppressed individuals, such as those with AIDS, leads to disseminated disease involving several organs, including the retina causes full-thickness retinal necrosis lesion is white with irregular granular borders, associated hemorrhage, and small "satellites" at the edge associated vitritis and anterior uveitis are usually mild SYPHILIS sexually transmitted desesase, G- bacterium Treponema pallidum eye affected during secondary and tertiary syphillis ocular manifestation – anterior uveitis ( granulomatous and nongranulomatous ), chorioretinitis, necrotizing retinitis, retinal vasculitis, intermediate uveitis and panuveitis many patient with ocular signs do not have systemic signs Th : penicillin G, BORELIOSIS tick-borne infection spirochaete Borrelia Burgdorferi symptoms – neurologic, cardiac, skin manifestation ocular involvement – in the second and late stage – any of the ocular structures Th: ATB OCULAR TUBERCULOSIS airborne infection caused by Mycobacterium tuberculosis, most commonly affects the lungs, although extrapulmonary manifestations are not uncommon histologically, tuberculous lesions are characterized by caseating granuloma intraocular tuberculosis result from hematogenous spread of the bacilli Tubercular decay has been found in the spines of Egyptian mummies OCULAR TUBERCULOSIS The most common presentation is posterior uveitis followed by anterior uveitis and panuveitis, tubercular retinal vasculitis is also common and is associated with vitreous infiltrates, retinal hemorrhage, neovascularization, and neuroretinitis The most common is multiple choroidal tubercles, which appear as small grayish nodules in the posterior pole Th: antituberculous th TOXOPLASMOSIS most common cause of posterior uveitis Toxoplasma gondii acquired – contaminated watter or undercooked meat spread by haematogenous dissemination – muscles, brain, retina clinical picture – necrotizing retinitis – self-limited, progressively resolves, leaving scar recurrences – unpredictable in immunosuppressive patient – multifocal, progressive Th: pyrimethamine, clindamicin, .. + KS – reducing the inflammatory reaction TOXACARIASIS Toxocara canis, cati usually – children the soil of parks and playgrounds is commonly contaminated with the eggs larvae migrate through the intestine wall to the blood, encystes in various tissues ( eye, brain, liver,..) ocular finding – granuloma death of the larva leads to severe intraocular inflamation Th: steroids FUNGAL UVEITIS uncommon causative organism – Candida, Aspergillus, cryptococcus, fusarium progresive intraocular inflamation immunocompromised or organ transplant patient Th : Amphotericin-B vitrectomy BENIGN TUMORS IRIS NEVUS CHOROIDAL NEVUS MALIGNANT TUMORS IRIS MELANOMA uveal melanoma is a malignant neoplasm that arises from neuroectodermal melanocytes within the choroid, ciliary body, or iris it is the most common primary malignant intraocular neoplasm of white adults metastasize hematogenously - liver CHOROIDAL MELANOMA Choroidal melanoma CHOROIDAL METASTASIS QUESTIONS AND DISCUSSION THANK YOU FOR YOUR ATTENTION !