* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download DELIRIUM - joshcorwin.com
Survey
Document related concepts
Transcript
Confusion, Delirium and
Dementia
Samira Khazravan, M.D.
Geriatric Fellow
Department of Geriatrics
Mary Immaculate Hospital
DELIRIUM
“Acute Confusional State”
DELIRIUM
Word delirium is derived from Latin term meaning "off
the track“.
Not a disease but a syndrome with multiple causes that
result in a similar constellation of symptoms.
The clinical hallmarks are ed attention span & a
waxing & waning type of confusion.
A transient, usually reversible, impairment of
consciousness with a ed ability to focus, sustain or
shift attention.
Should be treated as a medical emergency (early
diagnosis & resolution of symptoms are correlated with
the most favorable outcomes).
CRITERIA FOR DIAGNOSING
DELIRIUM
A ∆ in cognition or development of a perceptual
disturbance that is not better accounted for by a
preexisting, established or evolving Dementia.
Develops over a short period of time & tends to
fluctuate during the course of the day.
There is evidence that the disturbance is caused by
a medical condition, intoxication or med use.
There is no clear evidence of any underlying
pathologic process.
EPIDEMIOLOGY
14-56% of hospitalized elderly patients.
Delirium is present in 10-22% of elderly patients at the time of
admission, with an additional 10-30% of cases developing after
admission.
found in 40% of patients admitted to ICU.
Extremely common among nursing home residents.
Can occur at any age.
MC in pts who are elderly & have compromised mental status.
ed risk in pts w/dementia (2/3 of cases of delirium occur in pts
w/dementia).
Delirium due to physical illness is MC among very young & those
older than 60 years.
Delirium due to drug & alcohol intoxication or withdrawal is most
frequent in persons aged mid teens to the late 30s.
RISK FACTORS
Advanced age
Dementia
Functional impairment in ADLs
Medical co morbidity
History of alcohol abuse
♀ > or < ♂
MC whites than in other races
Sensory impairment – decreased vision & hearing
Acute cardiac/pulmonary events
HIV/AIDS
MORBIDITY/MORTALITY
10-fold risk of death.
3-5-fold increase risk of nosocomial complications.
Poor functional recovery & ed risk of death up to 2 years
Some causes of delirium (Delirium Tremens,
Severe Hypoglycemia, CNS infx, Heat stroke, Thyroid
storm) may be fatal or result in severe morbidity if
unrecognized & untreated.
With some exceptions, such as OD of TCAs, drug
intoxications generally resolve fully with supportive care.
PATHOPHYSIOLOGY
Exact pathophysiological mechanisms unclear.
The main hypothesis is reversible impairment of cerebral
oxidative metabolism & multiple NT abnormalities
(Acetylcholine, Dopamine, Serotonin, GABA)
Postulated mechanisms:
– Interruption of BBB
– Inflammatory mechanism [cytokines (interleukin-1 &
6) are ed following infx, inflammation, toxic insults,
head trauma & ischemia]
– Stress rxn mechanism [psychosocial stress and sleep
deprivation facilitate the onset of delirium].
ETIOLOGY Intracranial causes
Neurodegenerative
– Dementia w/Lewy bodies [only dementia that features
transient episodes of impaired consciousness as a typical
feature].
-No other dementias feature impairment of consciousness
unless complicated by a delirium (i.e. 2° to infx, anoxia,
etc).
ETIOLOGY Intracranial causes
Space-occupying lesions
– Tumor
– Cyst
– Abscess
– Hematoma
Head injury (esp. Concussion)
ETIOLOGY
INTOXICATION
– Alcohol (Delirium tremens, Wernicke-Korsakoff
encephalopathy).
– Sedative-Hypnotic use/abuse.
Poisons
Heavy metals (Lead, Mercury, Manganese)
Carbon monoxide
ETIOLOGY Drugs (ingestion or
withdrawal)
– Amphotericin B
– Anticholinergics
– Anticonvulsants
– Antidepressants
– Antihistamines
– Antihypertensive drugs [–
–
–
–
blockers]
Antiparkinsonian drugs
Antipsychotics
Cannabis
H2 Blocker (Cimetidine)
–
–
–
–
–
–
–
–
–
–
Dopaminergic agents
Disulfiram
Digoxin
Insulin
Lithium
Opiates
Phenytoin
Salicylates
Steroids
Sedatives (barbiturates
& benzodiazepines)
– TCAs
ETIOLOGY Intracranial causes
Infx
– Meningitis & Encephalitis (Bacterial, Viral, Fungal,
Parasitic or Tuberculosis organisms)
– Neurosyphilis
– Sepsis
Epilepsy
Cerebrovascular disorders
– TIA
– Cerebral thrombosis or Embolism
– Intracranial or SAH
– HTNive Encephalopathy
Vasculitis (e.g. From SLE)
ETIOLOGY Metabolic & endocrine
– Electrolyte
–
–
–
–
–
–
disturbances (Na+,
Mg2+, Ca2+)
Acid-Base D/o
Renal Failure &
Uremia
Hepatic
encephalopathy
Hypoglycemia (DM)
DKA
Insulinoma
– Thyrotoxicosis
– & thyroidism
– &
–
–
–
–
parathyroidism
&
adrenocorticism
(Cushing’s syndrome,
Addison’s disease)
Pheochromocytoma
Hypopituitarism
Wilson’s disease
ETIOLOGY
Nutritional Deficiencies
– Thiamine (Wernicke’s encephalopathy)
– Vitamin B12 (Pernicious Anemia)
– Vitamin B1 (Beriberi)
– Folic acid
– Niacin
Anoxia
– Respiratory failure (Hypoxia/Hypercarbia)
– Heart failure
MI, A. Fib
ETIOLOGY
Neoplasms (1 or metastatic lesions of
CNS; CA induced HyperCa2+)
Degenerative disease
– Alzheimer’s, Pick’s Dz, Multiple Sclerosis,
Parkinsonism, Huntington’s chorea, Normal
Pressure Hydrocephalus)
ETIOLOGY
Major
causes of delirium – HIDE
– Hypoxia
– Infections
– Drugs
– Electrolyte disturbances
SIGNS & SYMPTOMS
Usually acute onset
Fluctuating levels of consciousness (impairment
usually least in AM)
Perceptual disturbances (hallucinations or
illusions)
Impaired consciousness:
– Reduced awareness of environment clouding of
consciousness coma
– Reduced ability to sustain attention (easily
distracted)
SIGNS & SYMPTOMS
Impaired cognitive function
– Impaired STM (1° memory) & recent memory.
– Disoriented to time & often place [orientation
to self seldom lost].
– Language abnormalities [rambling, incoherent
speech & impaired ability to understand]
common.
SIGNS & SYMPTOMS
Perceptual & thought disturbance
– Ranging from misinterpretations (e.g. A door
slamming is mistaken for an explosion)
illusions (e.g. A crack in the wall is perceived
as a snake) hallucinations (especially visual)
Psychomotor abnormalities
– Patients may be hyper or hypoactive or
fluctuate from one to the other
– May also have an enhanced startle reaction
SIGNS & SYMPTOMS
Sleep-wake cycle disturbance
– Daytime drowsiness night-time hyperactivity
complete reversal of normal cycle
– Nightmares of delirious patients may continue as
hallucinations after awakening
Mood disturbance (Emotional Liability)
– Depression, euphoria, anxiety, anger, fear & apathy
– Lack of initiative, impaired impulse control, inability
to reason thru problems, confabulation
A physical illness should always be ruled
out whenever a patient presents with
prominent visual hallucinations because
patients with schizophrenia & other
functional psychotic disorders usually
experience auditory hallucinations.
DIFFERENTIAL DIAGNOSIS
Dementia
Primary psychiatric illnesses – Depression, Mania,
Schizophrenia.
Sundowning (mild to mod delirium @ night—MC in pts
w/preexisting dementia & may be precipitated by
hospitalization, drugs & sensory deprivation)disturbance
in circadian rhythm.
Focal syndromes – Wernicke’s aphasia, Anton’s syndrome
& Bi-frontal lesions.
Non-convulsive status.
DIFFERENTIAL DIAGNOSIS
Delirium often is unrecognized or
misdiagnosed & commonly is mistaken for
dementia, depression, mania, an acute
schizophrenic reaction or part of old age
(patients who are elderly are expected to
become confused in the hospital).
FEATURE
DELIRIUM
ONSET
Acute
DURATION
Hours –
weeks
Fluctuating
COURSE
CONSCIOUSNESS
PERCEPTUAL
DISTURBANCE
SLEEP-WAKE CYCLE
Impaired
Common
Disrupted
PROGNOSIS
Potentially
reversible
PRIMARILY AFFECTS Attention
MEDICAL
EMERGENCY?
Yes
DEMENTIA
Gradual
Months – years
Progressive
deterioration
Normal
Occurs in late
stages
Usually normal
Not reversible
Memory
No
DIAGNOSIS
Under-recognition is a major problem – nurses recognize &
document <50%; DSM-IV criteria is precise but difficult to apply.
History & Physical – focus on time course of cognitive changes,
especially their association w/other symptoms or events; Note
recently started meds, overdose, alcohol use, previous history,
concurrent medical problems, signs of organ failure & infx (occult
UTI is common in elderly), general medical evaluation, neurologic
& mental status examination.
Remember: Delirium is not a final diagnosis: this syndrome
indicates the presence of a very serious medical condition that
should be managed on medical not psychiatric, ward.
DIAGNOSIS
Any pt who presents w/AMS needs a complete PE, w/particular attn
to:
– General appearance (unkempt, tattooed &/or malnourished) may
suggest the possibility of drug or alcohol abuse)
– Vital signs
– Hydration status
– Evidence of physical trauma
– Evidence of neurological signs
The delirious or obtunded patient should be evaluated for Pupillary,
Fundoscopic & extraocular abnormalities; nuchal rigidity; thyroid
enlargement & heart murmurs or rhythm disturbances.
DIAGNOSIS
Other clues to etiology on PE:
– A pulmonary exam wheezing, rales or absent breath
sounds
– An abdominal exam Hepato/Splenomegaly
– A cutaneous exam rashes, icterus, petechiae,
ecchymosis, track marks or Cellulitis (often hidden under
clothing, particularly pants & socks; checking these areas
in pts with diabetes is critical; any serious infx can lead
to mental status ∆s)
CLUES TO DIAGNOSIS
Smell for alcohol
Musty odor of Fetor Hepaticus
Fruity smell of DKA
Icterus &/or asterixis liver failure w/ serum ammonia
Agitation & tremulousness sedative or A/C withdrawal
Fever infx, heat illness, thyroid storm, ASA toxicity or
extreme adrenergic overflow of certain drug overdoses &
withdrawal syndromes (Esp. delirium tremens)
Extreme hyperthermia (w/pinpoint pupils) pontine strokes
BP = common in delirium b/c of resulting adrenergic
overload
Hemotympanum, battle sign, raccoon eyes or otorhinorrhea
basilar skull fracture (2° to occult head trauma)
DIAGNOSIS
A rapid RR DKA (Kussmaul respiration), sepsis, stimulant
drug intoxication & ASA OD
A slow RR narcotic OD, CNS insult or various sedative
intoxications
A rapid PR fever, sepsis, dehydration, thyroid storm & cardiac
dysrhythmias & stimulants, anticholinergics, quinidine,
theophylline, TCAs or ASA OD
A slow PR ICP, asphyxia, complete heart block, CCBs,
Digoxin & beta-blockers
Pupillary dilation intoxication w/ hallucinogen, amphetamine,
cocaine or anticholinergic med
Pupillary constriction narcotic intoxication
Pupillary inequality late sign of uncal herniation
A funduscopic examination:
– Loss of venous pulsations early ICP elevation
– Papilledema severe ICP
DIAGNOSIS -- Special cases:
In pts w/delirium & severely BP, check ocular fundi for
arteriolar spasm, disc pallor, papilledema, flame
hemorrhages & exudates ( Malignant HTN).
In pregnant pts w/diastolic pressure >75 mm hg in 2nd
trimester or >85 mm hg in 3rd trimester Pre-eclampsia
(Hyperreflexia, Edema, Proteinuria).
In pts w/HTN & Bradycardia ICP
With Delirium & Hypotension dehydration, diabetic
coma, hemorrhage due to trauma, aneurysmal rupture, GI
bleeding, adrenergic depletion (2° to cocaine, amphetamine
or TCA OD) & Addisonian crisis (particularly in steroid
dependent pts).
DIAGNOSIS
A brief bedside neurologic exam, to include mental
status testing, is essential for workup of delirium
when a rapidly treatable cause (hypoglycemia or
narcotic OD) is not immediately apparent
The mini-mental status examination (MMSE) (a
formalized way of documenting severity & nature of
mental status ∆s)
In addition, or as an alternative to the MMSE,
correctly drawing the face of a clock (to include the
circle, numbers & hands) is a sensitive test of
cognitive function
Other simple screening tests include "serial 7's,"
LABORATORY/RADIOLOGICAL
CBC, electrolytes, BG levels, BUN/Cr
Also helpful – UA, LFTS (serum ammonia & PT), toxicology
screen, ABG, CXR, O2 Sat & cultures
Consider: Vitamin B-12 & Folate levels, VDRL test (r/o
Neurosyphilis) & thyroid function studies
Head CT scan [done b/f LP to r/o CNS infx, trauma, CVA, SAH,
hematomas, toxoplasmosis or abscess (especially in pts w/HIV
who present w/H/A)]
LP (CSF studies including India ink prep & VDRL)
Plain abdominal x-ray swallowed bags of drugs ("body
packing") or radiodense substances (iron tablets)
EKG (MI or a. fib; low voltages Hypothyroidism &
pericardial effusion; Tachycardia, widened QRS or prolonged QT
interval TCA overdose)
MANAGEMENT
ABC’s + Normalize fluid & electrolyte status
Provide Thiamine when administering glucose [or else may lead to acute
Wernicke syndrome (ataxia, confusion, oculomotor palsies in the setting of
malnutrition)]
Physical or pharmacologic restraints (may be necessary to prevent pts from
harming self or others)
Low dose Haloperidol (Typical Antipsychotic doc for severe agitation,
acute psychosis & severe delirium when no CIs exist) [sedative qualities +
effect on DA-Ach balance; Assess for akathisia & EPS; Avoid in elderly
w/parkinsonism; in ICU, monitor for QT prolongation, torsades,
neuroleptic malignant syndrome & withdrawal dyskinesias; antidote:
Dantrolene]
Avoid sedative meds if possible [use Benzodiazepines Lorazepam (Ativan)
-- doc in ED (if unable to control a dangerous patient; may obscure the
MMSE)]
Treat underlying cause
Multi-factorial approach is most successful
MANAGEMENT
Highly distressing for pts & anxiety provoking for medical ward
staff.
Hospitalization is essential.
To limit confusion, foster trust & provide reassurance, try to ensure
that pt is nursed by same staff consistently.
Maximize visual acuity (e.g. Glasses, appropriately lit
environment) & hearing ability (e.g. Hearing aid, quiet
environment) to avoid misinterpretation of stimuli.
Involve friend or family member to remain w/pt to help comfort &
orientate them.
Avoid complications of delirium – remove indwelling devices
ASAP, prevent or treat constipation, urinary retention & encourage
proper sleep hygiene.
COURSE & PROGNOSIS
Average duration of delirium is 7 days
Inpatients who develop delirium have an ed
mortality, with elderly pts having up to a 75%
chance of dying during that admission
Delirium is fully reversible in most cases with
proper recognition & treatment of the etiology
Failure to dx & manage delirium is costly, lifethreatening & can lead to loss of function
DEMENTIA
WHAT IS DEMENTIA?
An acquired syndrome of decline in
memory and other cognitive functions
sufficient to affect daily life in an alert
patient
Progressive and disabling
NOT an inherent aspect of aging
Different from normal cognitive lapses
Dementia
DSM IV criteria:
Development of cognitive deficits manifested by both
-impaired memory
-aphasia, apraxia, agnosia and disturbed executive
function
Significantly impaired social and occupational
function
Gradual onset and continuing decline
Not due to CNS and other physical or psychiatric
conditions
Prevalence
10% percent of persons over age 70
20 to 40% of individuals over age 85
Affects more than 4 million Americans
Costs more than $50 billion annually
Causes of Dementia & the
differential diagnosis:
Alzheimer’s disease
Vascular (multi-infarct) dementia
Dementia associated with Lewy bodies
Delirium
Depression
OTHER:
ETOH, exposure to heavy metals (arsenic, antimony, bismuth)
Parkinson’s disease, Pick’s disease, frontal lobe dementia
Infectious diseases: These infections may be caused by viruses
(HIV, viral encephalitis); spirochetes (Lyme disease,
neurosyphilis); or prions (Creutzfeldt-Jacob disease)
Abnormal brain structure: Hydrocephalus, subdural hematoma
Most common REVERSIBLE
causes
Hypothyroidism
Vitamin B-12
Folate deficiency
Dementia of depression
Drugs
Alcoholism
Assessment
History
Onset and Duration of the memory loss
A) Elderly person with slowly progressive memory loss
over several years AD
B) Change in personality with disinhibition and
intact memory may suggest FTD
C) History of sudden stroke with an irregular
stepwise progression suggests Multi-infarct
dementia
D) Rapid progression with rigidity and
myoclonus suggests CJD
Assessment (cont.)
E) Gait disturbances+memory problems+resting
tremors may suggest PD
F) Multiple sex partners or intravenous drug use
may indicate CNS infection
G) Hx of Recurrent head trauma suggests
Subdural Hematoma
H) Alcoholism Thiamine deficiency
I) Gait disturbances,urinary incontinence and
memory problems suggest NPH
Assessment (cont.)
Physical Examination
•
Cogwheel rigidity, bradykinesiaPD
•
Inability to initiate and coordinate stepsNPH
•
Myoclonic jerks are present in CJD
•
Hemiparesis or other focal neurologic deficits
MID
•
Dry cool skin,hair loss,bradycardia
Hypothyroidism
Cognitive assessment
MMSE
– most widely used screening exam
– used in assessment and follow up
– score interpretation depends on patients age
and education level
Clock drawing
– test of visuospatial skills
– draw numbers within a pre-drawn circle 3 inches
in diameter to make that circle look like the face
of a clock
– Normal score 0-3
– Dementia 4-7
MMSE
Orientation
Name: hospital/floor/town/state/country
5 (1 for each name)
Registration
Identify three objects by name and ask patient to repeat3
(1 for each object)
Attention and calculation
Serial 7s; subtract from 100 (e.g., 93-86-79-72-65)
5 (1 for each subtraction)
Recall
Recall the three objects presented earlier
3 (1 for each object)
Language
Name pencil and watch
2 (1 for each object)
Repeat "No ifs, ands, or buts“
1
Follow a 3-step command (e.g., "Take this paper,,
fold it in half and place it on the table")
3 (1 for each command)
Write "close your eyes" and ask patient to obey
written command
1
Ask patient to write a sentence
1
Ask patient to copy a design (e.g., intersecting pentagons)
1
TOTAL
30
Clock drawing
Cortical dementias
Alzheimer’s
Vascular
Diffuse Lewy body
Pick’s disease
Creutzfeldt-Jacob disease
Alzheimer’s
Slowly progressive dementing illness associated
with diffuse cortical atrophy, amyloid plaques and
neurofibrillary tangles
CLINICAL MANIFESTATIONS
• Progressive memory impairment (predominantly short term)
• Language impairment
• Complex deficits in visual and spatial abilities
• Acalculia
• Personality changes - progressive passivity to marked
hostility
• Increased stubbornness & suspiciousness
• Delusions
• Hallucinations
• Symptoms of depression and anxiety
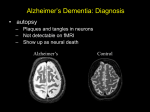
Alzheimer’s (cont.)
PLAQUES
Brain slice: left from
Alzheimer's Disease,
right from normal brain
TANGLES
CT SCAN
Alzheimer’s (cont.)
A.
MRI BRAIN NORMAL 86-year-old
male.
B. MRI BRAIN 77-year-old male with
Alzheimer's disease.
c. Fluorodeoxyglucose PET scans of a
normal control.
D. A patient with Alzheimer's disease.
Note that the patient
has decreased activity in the parietal
lobes bilaterally (arrows)
Alzheimer’s (cont.)
Management
– KISS (keep it simple and short)
– Maintain autonomy and independence
– Establish routines
– Safety issues: cooking, driving, community
services referral, discuss legal issues, caregiver
education
– Medications: donepezil, tacrine
Donepezil (ARICEPT)
Reversible cholinesterase (ChE) inhibitor
In Alzheimer's disease behavioral consequences (e.g., decline in
memory and learning) that are partially related to cholinergic
deficits
Used for the symptomatic management of mild to moderate forms of
Alzheimer's disease
DOSAGE
5 to 10mg qd
CONTRAINDICATIONS
Liver disease, alcoholism, peptic ulcer disease, chronic
obstructive pulmonary disease; and bradycardia
ADVERSE EFFECTS
N/V Diarrhea, Bradycardia Dizziness
Memantine (Namenda)
Non-competitive antagonist at N-methylD- aspartate receptors (NMDA)
Indicated for moderate to severe
Alzheimer’s disease.
Dose: 5 or 10 mg PO QD
Seizure disorder and renal disease are
contraindications.
HTN and Urinary Incontinence are the
adverse effects
Multi-infarct dementia
Results from an accumulation of discrete
cerebral strokes that produce disabling deficits
of memory, behavior, and other cognitive
abilities
CLINICAL MANIFESTATIONS
Stepwise deterioration
Focal neurologic deficits
Brain imaging shows multiple areas of stroke
Lewy Body Dementia
-Lewy bodies are intraneuronal inclusions that
stain with periodic acid-Schiff stain.
-In addition to chronic progressive dementia,
these patients often also have parkinsonian
features.
-Frequent fluctuations of behavior, cognitive
ability,and level of alertness may occur.
-No specific treatment
-No response to L- DOPA
Lewy Body (cont.)
Frontotemporal Dementia
Presents as disinhibition, apathy, or agitation.
Focal lobar atrophy of the frontal and/or temporal
lobes seen on MRI.
Pick's disease
Subcategory of FTD.
Microscopic findings include gliosis, neuronal loss,
and swollen or ballooned neurons, with Pick bodies.
Slowly progressive dementia ,bulimia, language
disturbance, emotional disinhibition, irritability,
and persistent aimless wandering,language
disturbance.
Huntington’s disease
-Autosomal dominant degenerative brain disorder.
-Chorea and behavioral disturbance.
-Attention, judgment, awareness, may be seriously
deficient at an early stage.
-No specific treatment.
-Adventitious movements and behavioral changes
may partially respond to phenothiazines.
Huntington’s (cont.)
Creutzfeldt-Jacob disease
Atypical infectious agents called “prions” cause
the disease.
It’s a transmissible neurodegenerative disorder.
Manifests in the sixth and seventh decade of life
as rapidly progressive dementia with myoclonus.
Minimal help with neuroimaging, EEG and CSF
analysis.
CSF protein 14-3-3, may be diagnostic
but the gold standard is………?
CJD cont….
Brain biopsy for premortem diagnosis.
Universal precautions are recommended for
routine patient care as the “prions” are very
resistant for routine disinfection methods.
The only known disease that can transmit through
corneal transplant and growth hormone
administration.
The disease in animals is called “bovine
spongiform encephalopathy”.
No effective treatment.
HIV dementia
Dementia in HIV occurs when the pt develops
AIDS(AIDS dementia complex).
-This is a diagnosis of exclusion based on
neuroimaging and spinal fluid analysis.
-Neuropsychiatric testing is helpful in
distinguishing from depression.
Clinical features…
Pts have difficulty with cognitive tasks and have
diminished motor speed. Dementia manifestations
may wax and wane with periods of lucidity and
confusion over the course of a day.
First clinical symptom may be deterioration in
hand writing.
Many pts will improve with effective antiretroviral
therapy.
Other types of dementia
Korsakoff’s syndrome
Wernicke’s encephalopathy
Parkinson’s disease
Chronic metal intoxications
Korsakoff’s syndrome
Caused by prolonged untreated thiamine deficiency
• Memory for new events is seriously impaired,
whereas memory of knowledge prior to the illness
is relatively intact
• Confabulation
-MRI Mammillary body atrophy
-No specific treatment
Wernicke’s encephalopathy
-Thiamine (vitamin B1)deficiency damages the
thalamus, mammillary bodies.
SYMPTOMS
Confusion
Ataxia
Diplopia
-Administration of parenteral thiamine may
reverse the disease.
Parkinson’s disease
Develops due to loss of dopaminergic neurons in
substantia nigra.
Approximately 20% of patients develop dementia.
CLINICAL MANIFESTATIONS
• Resting tremors
• Rigidity
• Bradykinesia
• Gait disturbances
Treatment with L-dopa neither accelerates nor
prevents this process.
Chronic metal intoxications
Lead poisoning
Mercury poisoning
Arsenic intoxication
Dialysis dementia syndrome
Dementia is part of normal
processing of age…
True?
False?
Dementia impairs physical
functioning of the individual…
True?
False?
Delirious patient may have
auditory hallucinations…
True?
False?
A person with dementia may
develop delirium…
True?
False?
A person with delirium will
develop dementia…
True?
False?
A 70 YO man comes and tells you that
he has been forgetting certain things
and has difficulty of recollecting some
names.
He is having dementia….?
True ? False ?
THANK YOU