* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Review of Reasoning Methods in Clinical Decision Support Systems
Survey
Document related concepts
Transcript
18th Telecommunications forum TELFOR 2010
Serbia, Belgrade, November 23-25, 2010.
Review of Reasoning Methods in Clinical
Decision Support Systems
Liljana Aleksovska - Stojkovska, Member, IEEE, Suzana Loskovska, Senior Member, IEEE
Abstract—Reasoning is a crucial task performed by the
inference engine of the clinical decision support systems,
which combines medical knowledge with patient specific data
and generates relevant decisions. There are different
reasoning methods, suitable for different knowledge
representations and application area. This paper reviews the
most common methods and describes how they are used in
real systems. Furthermore, it outlines the remaining
weaknesses of the reasoning mechanisms and provides
directions for future research and improvements.
Keywords — Clinical decision support systems, inference,
inference engine, reasoning methods
I. INTRODUCTION
inference can be defined as “act of using
reason to derive a conclusion from certain premises
using a given methodology, following the logical
definition” [1]. The reasoning process in medical
diagnostic is a complex process as it has to consider many
different facts, including the patient’s history, current
symptoms, test results, received therapies, possible
allergies and map these conditions to a list of possible
matching diagnoses. The importance of understanding this
process has been emphasized by the increasing interest in
the use of computers as an aid to medical diagnostic
processes [1]. When a physician is asked to describe the
medical diagnostic process, his explanation may be as
follows [1]. First, the case facts are obtained from the
patient’s history, medical examination and laboratory tests.
Second, evaluation is performed of the relative importance
of the different signs and symptoms. Third, to make a
differential diagnosis, list is created of all diseases with
reasonable resemblance to the specific case. Then, the list
is evaluated and the less relevant diseases are excluded
until the case can be fitted into a definite disease category.
This is obviously a simplified explanation of the
diagnostic process [1]. Physicians describe that often after
seeing the patient they have a “feeling” about the case,
R
EASONING or
Liljana Aleksovska – Stojkovska, MSc., 701 Huntington Commons
Rd. #214, Mount Prospect, IL, 60056, USA, (tel: 1-847-739-6485, email: liljana.a.stojkovska@gmail.com); curently PhD student at the
Faculty of Electrical Engineering and Information Technologies,
University „Ss. Cyril and Methodius“ – Skopje, Republic of Macedonia
Suzana Loskovska, PhD., University „Ss. Cyril and Methodius –
Skopje“, Faculty of Electrical Engineering and Information
Technologies, Karpos II, bb, 1000 Skopje, Republic of Macedonia, (tel:
+389 70 390 842, e-mail: suze@feit.ukim.edu.mk)
which may be a summary of the patient’s general
appearance, facial expression, how all facts fit together or
it may be a great resemblance to a previous case [1]. This
is especially true for the experts with long experience, who
have developed highly automated perceptual ability and
rapid recognition skills [2]. It is believed that the
physicians have tendency to generate hypotheses very early
in the process of solving a diagnostic problem and this is a
result of complex reasoning, which is performed
automatically without being aware of the different
reasoning methods that are applied [2].
Scientists have developed many different reasoning
mechanisms, which are available to be used by the
inference engine within the Clinical Decision Support
Systems (CDSS). However, even decades since the CDSSs
were initially introduced, there are still unresolved
problems and no single method has been found to answer
all questions. The main purpose of this paper is to review
the different reasoning methodologies and to provide
directions for future research and improvements.
The paper is organized as follows. Section 2 reviews
some of the most common reasoning methods. Section 3
describes how these methods are combined and used in
real decision support systems. Section 4 describes the
weaknesses of the reasoning mechanisms, followed by
Section 5, which provides ideas how some of these
problems can be solved. Finally, Section 6 concludes the
review.
II. REVIEW OF THE REASONING (INFERENCE) METHODS
Medical decision making can be viewed along a
spectrum, with categorical (or deterministic) reasoning at
one extreme and probabilistic (or evidential) reasoning at
the other [3]. The categorical reasoning uses an
appropriate set of predefined routines or rules, which apply
to the great majority of clinical situations [3]. A
categorical decision is simple to make, its appropriateness
is easy to judge and its result is unambiguous [3]. For
example: if the patient complains of pain on urination,
obtain urine culture and consider the possibility of urinary
tract infection [3].
Unfortunately, most of the medical decisions are not that
simple. For example, no simple rule exists for deciding
when to discharge a patient from intensive care unit after
suffering heart attack [3]. In this kind of situations,
decisions are made by careful consideration of all the
evidence, which means estimating the probability of all the
different facts that are included in the specific case [3].
1105
Following are some of the most common reasoning
mechanisms, along the scale between categorical and
probabilistic.
Rule-based reasoning is based on “if-then-else” rule
statements, which are viewed as patterns and the inference
engine searches for patterns in the rules that match patterns
in the data [4]. The rules reasoning can be forwardchaining, (data-driven), where the reasoning starts with
data or facts and looks for rules which apply to the facts
until a goal is reached or backward-chaining (goal-driven),
where the reasoning starts with a goal and look for rules
which apply to that goal until a conclusion is reached [4].
Case-based reasoning searches for commonly
occurring patterns among the stored various cases [7]. It is
used when the medical knowledge is difficult to be
modeled with the formal representation methods [4].
Crucial requirements for the success of this method are
good similarity measures and efficient ways of searching
for similar cases [7]. Advantage of case-based reasoning is
that similar clinical cases are often more convincing than
the theoretical medical knowledge, but, the difficulty to
measure the similarity between cases and the complex
retrieval process are disadvantages [4].
Model-based reasoning provides framework for
diagnosing an artifact by observing its manifested behavior
and comparing it to the predicted behavior of the artifact’s
model [8], [9], [10]. It assumes that if the model is correct,
all discrepancies between the observed and the predicted
behavior arise from the defects in the observed device
[10]. However, the real problem with this methodology is
that there is no guarantee that the model is correct and it is
challenging to come up with a right model, especially in
case of complex systems.
Bayesian reasoning is based on conditional
probabilities and predicts the posterior probability of
specific event given the occurrence of another event [5].
In context of CDSS, Bayesian network can be used to
compute the probabilities of the presence of possible
diseases given their symptoms.
Heuristic reasoning methods exploit the information
processing structure of the reasoning system and the
structure of the environment to produce reasonable
answers when knowledge and/or computational resources
for finding the perfect answer may not exist [6]. Heuristic
systems proposed for medical reasoning include statistical
methods, such as support vector machine (SVM) and least
square support vector machine (LSSVM) [4].
Semantic network is a declarative graphic
representation in patterns of interconnected nodes and arcs
that can be used to support automated systems for
reasoning about knowledge [7]. In CDSS, since most
medical knowledge involves uncertainties, it is difficult to
use a pure semantic network to make clinical inference [4].
Neural networks are a black box modeling technique
that model relationships by learning from historical data
and patterns recognition [4]. Advantage of neural networks
is that it is not necessary to understand the relationship
between input and output variables [4]. A disadvantage is
that their knowledge domain is very limited and they can
not explain their reasoning process, so most clinicians
don’t use them for reliability and accountability reasons.
Genetic algorithms are based on simplified
evolutionary processes using directed selection to achieve
optimal results. The selection algorithms evaluate
components of random sets of solutions to a problem. The
solutions that come out on top are then recombined and
mutated and run through the process again. This process is
continuously repeated till the proper solution is discovered.
Their advantage is that similar to the neural networks, they
derive their knowledge from patient data and the most
optimal solution can be achieved, but determining what is
the fittest solution is a challenge [4].
From this review it can be concluded that different
reasoning mechanisms have different advantages and
disadvantages and can be more or less suitable for specific
systems. The focus of research is to find appropriate ways
to combine these methods to create competent programs
which exhibit medical expertise [3]. It is common that
different reasoning methods are frequently combined, such
as: integration of rule-based and case-based reasoning,
integration of model-based with case-based reasoning [12].
III. INFERENCE MECHANISMS USED IN CDSS
This section provides examples how the reasoning
methods are used by the inference engines within CDSS.
INTERNIST is a computerized diagnostic program,
designed at the University of Pittsburgh in 1974, which
covers approximately 80 % of the diagnoses of internal
medicine [3], [13]. The INTERNIST database associates
every possible diagnosis Di a set of manifestations {Mj}. A
manifestation is a finding, symptom, sign, laboratory test
or another associated diagnosis. For every Mj listed under
Di two likelihoods are entered [3]:
• ESDi|Mj - Evoking Strength (ES) is the likelihood that if
Manifestation Mj is seen in a patient, its cause is Di. It
is assessed on a scale 0-5, where 5 is the maximal
likelihood, while 0 virtually means no support.
• FWMj|Di – Frequency Weight (FW) is the likelihood
that a patient with a confirmed diagnosis Di would
exhibit manifestation Mj. It is assessed on a scale 1-5,
where 1 means that the specific manifestation rarely
occurs in the disease, while 5 means that the
manifestation essentially occurs in all cases.
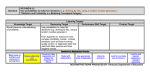
Fig. 1 shows how a Diagnosis and its Manifestations are
represented in INTERNIST.
1106
Disease profile for
ECHINOCOCCAL CYST <S> OF LIVER
ES
FW Symptom
1
2
COUGH
1
1
FECES LIGHT COLORED
0
2
FEVER
1
3
HEPATOMEGALY PRESENT
1
2
JAUNDICE
1
2
LIVER TENDER ON PALPATION
Fig. 1. Diagnosis and its Manifestations in INTERNIST
INTERNIST classifies all diagnosis in a disease
hierarchy, which is used during the diagnostic process for
determining a general diagnosis and the corresponding
specializations. INTERNIST identifies for each general
diagnosis a list of manifestations and computes their
corresponding Evoking Strengths and Frequencies. The
manifestations of the general diagnosis are common for
each of its specializations and the ES and FW are
respectively the maximum ES and the minimum FW of
that manifestation among the specializations [3]. The
diagnosis is active if there is at least one manifestation with
a non-zero ES. For each active hypothesis a score is
computed and the system focuses on the highest ranking
diagnosis [3]. The lower ranking diagnoses are categorized
in two groups: competing and complementary. The
diagnosis is complementary to the chosen one if the two
together account for more findings than either one alone,
otherwise it is competing [3]. The process of scoring,
ranking and partitioning is repeated after each new fact is
identified. INTERNIST uses combination of categorical
and probabilistic reasoning. The decision making is mostly
probabilistic. The hierarchic tree of diagnoses and the rule
for moving from general to specific diagnosis are
categorical.
MYCIN is a rule-based expert system designed to
diagnose and recommend treatment for certain blood
infections, developed in the mid-1970s by Ted Shortliffe
and colleagues at Stanford University [13]. It uses goaldirected backward-chaining reasoning, while trying to
determine if the patient is suffering from significant
infection, which should be treated and propose appropriate
therapy [3].
MYCIN’s knowledge base is composed of rules, with a
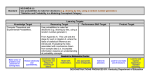
typical rule shown on Fig. 2.
param
context operation value
---------- ----------- ------------ -------(defrule 52
<--- rule #
if (site
culture
is
blood )
(gram
organism is
neg ) <--- remise/
(morphl organism is
rod )
condition
(burn
patient
is
serious)
then 0.4
<--- cf
(identity organism is pseudomonas ) <---conclusion
)
Fig. 2. A typical MYCIN rule
With each fact H in the database, MYCIN associates
measure of belief (MB) and measure of disbelief (MD),
which are numbers between 0 and 1 [14]. The difference
between these numbers gives the Certainty Factor (CF),
which ranges between -1 and 1 and is calculated with the
following formula [3]:
CFH = MBH - MDH
(1)
The value of every clinical parameter is stored by
MYCIN along with an associated certainty factor (CF),
which reflects MYCIN's "belief" that the value is correct
[14]. MYCIN uses confirmation formalism for computing
the certainty of multiple facts [3]. When the Rule S1 infers
the hypothesis H with measure of belief MBH|S1 and the
Rule S2 leads to the same hypothesis H with measure of
belief MBH|S2, the certainty for the hypothesis H is
calculated with the following formulas [3]:
MBH|S1,S2=0, if MDH|S1,S2=1
(2)
MBH|S1,S2= MBH|S1+ MBH|S2(1- MBH|S1), otherwise (3)
MDH|S1,S2=0,if MBH|S1,S2=1
(4)
MDH|S1,S2= MDH|S1+ MDH|S2(1- MDH|S1), otherwise (5)
The certainty factor of hypothesis when multiple rules
have contributed evidence to it, is calculated as in [3]:
CFH= MBH|S1,S2 - MDH|S1,S2
(6)
In case of multiple active hypotheses, their conjunction
and disjunction is calculated with these formulas [14]:
MBH1andH2=min(MBH1, MBH2)
(7)
MDH1andH2=max(MDH1, MDH2)
(8)
CFH1andH2=min(CFH1, CFH2)
(9)
MBH1orH2=max(MBH1, MBH2)
(10)
MDH1orH2=min(MDH1, MDH2)
(11)
CFH1orH2=max(CFH1, CFH2)
(12)
In addition to the rules, MYCIN also includes context
hierarchy, which plays smaller, but still important role in
the system’s operation [3]. Similar to INTERNIST,
MYCIN uses combination of categorical and probabilistic
methods. The rule-based knowledge presentation and
backward-chaining
are
purely
categorical
[3].
Probabilistic reasoning resides in calculation of measure of
belief, measure of disbelief and certainty factor [3].
IV. CRITIQUE AND ANALYSIS
As presented in this paper, there is a number of different
reasoning methodologies, which can be combined and used
within real clinical diagnostic systems. It has to be
admitted that choosing the right method or combination of
different methods to create an efficient inference engine,
well suited for its application area, still remains a
challenging task. This section analyses some of the
remaining problems, which need additional research and
solution.
Systems with broad domain, such as INTERNIST, have
inadequate criteria for deciding when the diagnosis is
complete [3]. The systems have no sense when the main
diagnostic problem is resolved and continue wasting time
and resources by exploring less and less suitable
hypotheses.
The initial strategy of the diagnostic systems is to use
every new finding as a trigger for discovering a possible
disorder, so new hypotheses are continually generated [3].
When an expected finding is requested to support one of
the leading diagnoses and when that finding is presented,
the system often generates a completely new hypothesis,
even though the finding is consistent with the diagnosis
being considered. Obviously, such sensitivity is needed to
a certain point, but it is preferred if the new hypothesis is
triggered only by evidence contradictory to the current
belief.
When multiple hypotheses are being considered, the
diagnostic systems are not very good at distinguishing the
different possibilities: the two hypotheses occurring
together but are unrelated, one hypothesis was caused by
1107
the first one or only one of the hypothesis is active but not
both [3], [15].
The medical reasoning necessarily involves uncertainty,
which mainly comes from the incomplete or imprecisely
specified knowledge about important facts that are
contributing to a decision. Therefore, effective methods
should be developed to handle the uncertainty in medical
reasoning. When solving complex problems where
multiple uncertain factors have to be considered, the
probabilistic models are necessary [3]. The number of
probabilities to be calculated is huge. For example, in a
system which considers 20 diseases and 50 symptoms,
there should be 1000 probabilities that the symptom j is
associated with the disease i [15]. On the other side, it was
observed from the experience that the experts, even the
most experienced ones, are extremely reluctant in engaging
in any type of numerical computation involving likelihood
of diagnosis or prognosis of treatment [3]. While doctors
can confidently make quick decisions about diagnoses or
treatment just from observing the patient or taking a quick
look at their medical facts, these hypotheses usually come
as a result of recognition or comparison with similar cases
from the past experience rather than from any formal
computation of probabilities.
Ongoing research must be performed in the direction of
these weaknesses to make the clinical decision support
systems as close as possible to the human experts.
V. DIRECTIONS FOR POSSIBLE IMPROVEMENTS
This section provides some ideas and directions for
future research, which may lead to resolving some of the
difficulties discussed previously.
Regarding the appropriate termination of the diagnostic
process, [3] proposes that the diagnosis needs to be only as
precise as is required by the next decision to be taken by
the doctor. This can be achieved by applying the Bayesian
methods which can compare the cost of the new
information to its expected benefit and ignoring the
remaining possible diagnoses, which are irrelevant [3],
[15]. For this purpose a termination probability is
calculated and if the disease attains a probability higher
than the termination probability, the further processing is
terminated and only the leading diagnoses with highest
probabilities are presented [15].
The diagnostic systems shall have mechanisms to check
if the newly presented fact is related to a currently
established diagnosis or an existing chronic illness [3]. For
example: in case of patient with a long history of sickle
cell anemia, who presents a new symptom of joints pain,
the system should not immediately raise a hypothesis that
the patient suffers from rheumatoid arthritis, but it should
realize that it is a reasonable consequence of already
known disease process [3]. This approach also may be
helpful in the complex cases where the patient is suffering
from more than one disease and the symptoms are
overlapping. Also, the diagnostic systems must be aware of
the ongoing trends of illnesses and epidemics, so in cases
when patient presents with symptoms of known infection
disease in the local community, the possibility of that
infection shall be immediately checked before any other
analysis are performed [15].
Regarding the problem with uncertainty and calculation
of the probabilities, statistical methods can be used to
obtain the likelihoods directly from the patient’s database.
It is believed that this approach would give much more
accurate numbers compared to the numbers provided by
the physicians.
VI. CONCLUSION
The inference engine represents the brain of the CDSS,
therefore selecting the right inference mechanisms is
crucial in determining the success of the entire system.
After the critical review of the existing reasoning methods
and their use within real CDSS, a conclusion can be drawn
that significant progress has been made theoretically and
practically. There are numerous reasoning methods
developed, which can be combined to get optimal results.
Additional research must be performed to improve these
methods and overpass the existing weaknesses.
CDSS promise to make a significant impact in the
medicine. However, because of the numerous limitations,
they have to be considered only as assistants to the human
experts rather then expected to replace them completely.
REFERENCES
[1]
[2]
[3]
[4]
[5]
[6]
[7]
[8]
[9]
[10]
[11]
[12]
[13]
[14]
[15]
1108
R.S. Ledley, L.B. Lusted, “Reasoning foundations of medical
diagnosis”, in Science, vol. 130, no. 3366, Jul. 1959, pp. 9-21.
V. L. Patel, G. J. Groen, “Knowledge based solution strategies in
medical reasoning”, in Cognitive Science, vol. 10, no. 1, Jan-Mar
1986, ISSN 0364-0213, pp. 91-116.
P. Szolovits, S. G. Pauker, in “Categorical and Probabilistic
Reasoning in Medical Diagnosis”, in Artificial Intelligence, vol.
11, no. 1-2, 1978, pp. 115-144.
G. Kong, D. L. Xu, J.B. Yang, The University of Manchester,
“Clinical Decision Support Systems: A Review On Knowledge
Representation And Inference Under Uncertainties”, in
International Journal of Computational Intelligence Systems,
vol.1, no.2, May 2008, pp. 159-167.
Charles River Analytics, Inc., “About Bayesian Belief Networks”,
for BNet Version 1.0, Last Updated April 22, 2008.
P. K. Paritosh, “The heuristic reasoning manifesto”, in Proceedings
of the 20th International Workshop on Qualitative Reasoning, 2006
J. F. Sowa, editor, “Principles of Semantic Networks”, Morgan
Kaufmann, Los Altos, 1991.
J. de Kleer, J. and B. C. Williams, “Diagnosis with behavioral
modes”, in Proceedings IJCAI-89, Detroit, MI (1989) pp. 104-109.
J. de Kleer, and B.C. Williams, “Diagnosing multiple faults”,
Artificial Intelligence, vol. 32, 1987, pp. 97-130.
R.
Davis,
and
W.
Hamscher,
“Model-based
reasoning:Troubleshooting”, in Exploring artificial intelligence,
edited by H.E. Shrobe and the American Associationfor Artificial
Intelligence, (Morgan Kaufman, 1988), pp. 297-346.
V. Novacek, “Inference Support for Ontology Acquisition”,
Dissertation Thesis Topic, Faculty of Informatics, Masaryk
University, Czech Republic, Jan 3, 2007.
C. Marling, E. Rissland, A. Aamodt, “Integrations with case-based
reasoning”, in The Knowledge Engineering Review, vol. 00:0,
2005, pp.1–4, Cambridge University Press.
Open Clinical: Decision Support Systems, Mar 2010
Available: http://www.openclinical.org/dss.html
Exert Systems Case Studies: MYCIN
Available:
http://www.computing.surrey.ac.uk/ai/PROFILE/mycin.html
G. A. Gorry, J. P. Kassirer, A. Essig, and W. B. Schwartz,
“Decision Analysis as the Basis for Computer-Aided Management
of Acute Renal Failure”, in The American Journal of Medicine,
vol. 55, Oct. 1973, pp.473-484.