* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Hypertension
Pharmacogenomics wikipedia , lookup
NMDA receptor wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Toxicodynamics wikipedia , lookup
Pharmacognosy wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Norepinephrine wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Drug interaction wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Psychopharmacology wikipedia , lookup
Neuropharmacology wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
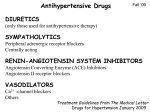
Antihypertensives or How not to blow your cork Background Cardiovascular pharmacology must always deal with two problems 1. Treating the disease state (e.g. reducing elevated blood pressure) 2. Accounting for the body’s homeostatic response to the treatment Individual variation in response, and probable drug interactions, will dictate the correct regimen of drugs to be administered Goal is to develop regimen using fewest drugs at lowest effective doses Reduces number and severity of side effects Increases patient compliance Hypertension Defined as elevation of arterial blood pressure above a normal value (120/80 mmHg). Highest risk factor associated with cardiovascular disease risk doubles with each 20 mm Hg increase in systolic bp over 140 mm Hg Most cases of hypertension (90%) are due to unknown etiology called essential hypertension Normal increase in bp with age (most cases diagnosed in middle age) Note: for this class BP = AP Hypertension is asymptomatic but may increase risk of other pathologies: Atherosclerosis Coronary artery disease Congestive heart failure Diabetes Insulin resistance Stroke Renal disease Retinal disease (easiest condition to diagnose) Recall: Regulation of blood pressure due to combination of Renin-angiotensin-aldosterone system Sympathetic nervous system Vasopressin (ADH) system Fluid retention/excretion by the kidney Note: the most effective antihypertensive drug regimens will impair the function of one or more of the above systems Compensatory mechanisms counteracting decreased blood pressure Classes of Antihypertensive Drugs 1. 2. 3. 4. 5. 6. 7. β blockers Peripherally acting sympatholytics Centrally acting sympatholytics (Diuretics) Angiotensin inhibitors Calcium channel blockers Direct vasodilators Figure 12-2 Summary of sites and mechanisms of action antihypertensives Stages of Hypertension Heart failure Angina Post-myocardial infarction Extensive coronary artery disease Diabetes Chronic kidney failure Recurrent stroke prevention Mechanisms of Action: Diuretics Will talk about specifics later but generally reduce blood volume by decreasing electrolyte, and thus water, reabsorption in the kidney (increase urine excretion) Causes reduced plasma volume which decreases CO, which lowers BP Diuretics amiloride Thiazides* burnetanide chlorthalidone eplerenone furosemide (also used in race horses, altitude sickness) indapamide metolazone spironolactone triamterene Mechanisms of Action: Angiotensin Inhibitors Angiotensin converting enzyme (ACE) inhibitor blocks conversion of angiotensin I to angiotensin II Angiotensin receptor blockers Reversibly bind to the Ang. I subtype of Ang. II receptors in blood vessels reduce physiological effect of Ang. II Note: both above have similar antihypertensive effect Angiotensin Inhibitors ACEs captopril enalapril lisinopril benazepril ramipril Angiotensin receptor blockers losartan valsartan candesartan telmisartan Mechanisms of Action: Drugs affecting the SNS – Adrenergic β, α receptor antagonists Many types of β blockers All competitively antagonize the effects of epinephrine and norepinephrine on β1 –adrenergic receptors in the heart, and renin-secreting cells of the kidney α receptor antagonists work only by blocking α1 receptors on vascular smooth muscle Mechanisms of Action: Drugs affecting the SNS – Sympatholytics CNS active Work by reducing the firing rate of sympathetic nerves Mediated by activation of α2-adrenergic receptors in the CNS but exact site is unclear Enter brain after absorption into bloodstream Peripherally acting Interfere with norepinephrine release from sympathetic nerve terminals May inhibit formation of catecholamines Adrenergic receptor antagonists β-blockers propanolol atenolol sotalol pindolol labetalol Carvedilol α1 receptor antagonists clonidine α-methyldopa guanfacine guanabenz Reserpine – 1st widely used antihypertensive Mechanisms of Action: Ca2+ Channel Blockers All excitable tissue contains voltage-dependent Ca2+ channels Inhibit inward movement of Ca2+ through specific (L-type) voltage-dependent Ca2+ channels This type of channel prevalent in cardiac and vascular smooth muscle When Ca2+ channels are inactivated, Ca2+ is pumped out of cell, actin dissociates from myosin and muscle relaxes, opening vascular lumen and decreasing resistance, which decreases BP Major effect is on coronary and peripheral arterioles Ca2+ channel blockers Verapamil (1st one used to treat hypertension) nifedipine diltiazem Mechanisms of Action: Direct vasodilators Most powerful antihypertensive drugs May cause strong compensatory reactions to bring BP back up Fluid retention Increase in renin-release heart rate contractility Usually used only in severe hypertension or for patients not responding to other antihypertensives Direct vasodilators Hydralazine Minoxidil Pinacidil Diazoxide Clinical considerations: diuretics Usually well tolerated, relatively cheap, and work as well as other methods They are especially effective in AfricanAmericans At initial treatment urinary excretion increase significantly but after several days returns close to normal, and BP remains depressed Clinical considerations: angiotensin inhibitors Most effective in patients with elevated plasma renin levels (but this condition is rare) Still effective in hypertensive patients with normal or even low levels of renin Useful for treating hypertension associated with other cardiovascular risk factors, like heart failure, stroke, myocardial infarctions, diabetes, and kidney disease Clinical considerations: SNS drugs The long-term decrease in CO is usually most responsible for lowering BP For some patients CO returns to normal as TPR decreases decreased BP continues β–blockers also inhibit renin release which contributes significantly to decreased BP, especially if renin levels are elevated Effect on two different systems causes β–blockers to often be used in combination with other antihypertensives (direct vasodilators, α1 adrenergic receptor blockers) because get three types of effects with only two drugs β–blockers may also counteract reflex compensatory responses (that increase CO) caused by these other drugs Clinical considerations: SNS drugs (con’t) Peripheral α1 adrenergic receptor blockers (prazosin, doxazosin) reduce TPR may cause fluid retention may then need to give diuretics to counteract Clinical considerations: 2+ Ca channel blockers All excitable tissue contains receptors for Ca2+ channel blockers but not all tissue affected equally Dependence of tissue on exogenous Ca2+ dictates sensitivity to blockers High in cardiac tissue (especially AV node), lower in skeletal muscle Some may be contraindicated due to other disease states or if using specific drugs Example - do not use verapamil in cases of heart failure associated with increased TPR will slow down an already poorly pumping heart Example - do not use certain β-blockers in combination with Ca2+ channel blockers in heart failure Drugs for hypertensive emergencies May have to reduce BP quickly but temporarily Unexpected side effects of other drugs Side effects of illegal drugs Accidental poisoning Above may cause severe tachycardia can reduce BP (and HR) by i.v. infusion of nitroprusside Full effect in seconds Recovery from effect within a few minutes Or repeated low-dose i.v. injections of diazoxide Full effect in 1 to 5 minutes Recovery within a day Treatment of Hypertension and see Table 12-1