* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
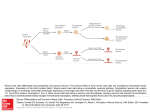
Download Guidance cues involved in the development of the peripheral
Survey
Document related concepts
Transcript
Autonomic Neuroscience: Basic and Clinical 112 (2004) 1 – 14 www.elsevier.com/locate/autneu Review Guidance cues involved in the development of the peripheral autonomic nervous system H.M. Young *, R.B. Anderson, C.R. Anderson Department of Anatomy and Cell Biology, University of Melbourne, 3010 VIC, Australia Received 9 December 2003; received in revised form 25 February 2004; accepted 26 February 2004 Abstract All peripheral autonomic neurons arise from neural crest cells that migrate away from the neural tube and navigate to the location where ganglia will form. After differentiating into neurons, their axons then navigate to a variety of targets. During the development of the enteric nervous system, GDNF appears to play a role in inducing vagal neural crest cells to enter the gut, in retaining neural crest cells within the gut and in promoting the migration of neural crest cells along the gut. Sema3A regulates the entry of extrinsic axons into the distal hindgut, netrin-DCC signaling is responsible for the centripetal migration of cells to form the submucosal ganglia within the gut, Slit – Robo signaling prevents trunk level neural crest cells from entering the gut, and neurturin plays a role in the innervation of the circular muscle layer. During the development of the sympathetic nervous system, the migration of trunk neural crest cells through the somites is influenced by ephrin-Bs, Sema3A and F-spondin. The migration of neural crest cells ventrally beyond the somites requires neuregulin signaling and the clumping of cells into columns adjacent to the dorsal aorta is regulated by Sema3A. The rostral migration of cells to form the superior cervical ganglion (SCG) and the extension of axons along blood vessels involves artemin signaling through Ret and GFRa3, and the entry of sympathetic axons into target tissues involves neurotrophins and GDNF. Relatively little is known about the development of parasympathetic ganglia, but GDNF appears to play a role in the migration of some cranial ganglion precursors to their correct location, and both GDNF and neurturin are involved in the growth of parasympathetic axons into particular targets. D 2004 Elsevier B.V. All rights reserved. Keywords: Guidance cues; Peripheral; Autonomic nervous system 1. Introduction All peripheral autonomic neurons (sympathetic, parasympathetic and enteric) arise from neural crest cells that migrate away from the neural tube and navigate to the location where ganglia will form. After differentiating into neurons, their axons then navigate to a variety of targets. These processes rely upon molecules that are attractive or repulsive to the migrating cells or growth cones of growing axons. In this review, we first briefly summarize the classes of guidance cues that are involved in neural crest cell migration and axonal navigation during the development of the autonomic nervous system. We then describe in detail how different guidance molecules act at different developmental stages during the development of the enteric, sympathetic and parasympathetic nervous systems. A summary * Corresponding author. Tel.: +613-8344-0007; fax: +613-9347-5219. E-mail address: h.young@unimelb.edu.au (H.M. Young). 1566-0702/$ - see front matter D 2004 Elsevier B.V. All rights reserved. doi:10.1016/j.autneu.2004.02.008 of the guidance cues involved in the development of autonomic neurons and their roles is shown in Table 1. 2. Neural guidance cues 2.1. ‘‘Classical’’ neural guidance molecules Enormous progress has been made in the past few years in identifying molecules that function as attractive or repulsive cues to guide migrating neural cells and growing axons during development. Axon guidance and directed neural migration (collectively called ‘‘neuronal navigation’’ by Song and Poo, 2001) use common guidance molecules— netrins, semaphorins, slits and ephrins—and it appears that members of all of these major families of neural guidance molecules play some role in autonomic neuron development. Neural guidance molecules and their receptors are expressed in precise spatial and temporal patterns during development. 2 H.M. Young et al. / Autonomic Neuroscience: Basic and Clinical 112 (2004) 1–14 Table 1 Summary of signalling pathways that influence migration and axon guidance during the development of different regions of the peripheral autonomic nervous system Enteric Guidance cue Proposed role in neural guidance References GDNF/GFRa1/Ret Promote migration of vagal neural crest cells into and along the gut, retain neural crest cells within the gut Influence entry of extrinsic axons into the hindgut Induce secondary migration from myenteric to submucosal region of the gut Induce growth of axons into circular muscle layer Prevents trunk level neural crest cells from entering the gut Prevent trunk neural crest cells from entering caudal half of each somite Young et al. (2001); Natarajan et al. (2002); Iwashita et al. (2003) Shepherd and Raper (1999) Jiang et al. (2003) Sema3A/neuropilin-1 Netrins/DCC Sympathetic Neurturin/GFRa2/Ret Slit/Robo EphrinBs/EphB3, Sema3A/neuropilin-1, F-spondin Neuregulin/ErbB2, ErbB3 Sema3A/neuropilin-1 Artemin/GFRa3/Ret NGF/TrkA Parasympathetic Otic ganglion Ciliary ganglion GDNF/GFRa1/Ret GDNF/GFRa1/Ret Heuckeroth et al. (1999); Rossi et al. (1999) De Bellard et al. (2003) Krull (2001); Halloran and Berndt (2003) Promote migration ventral to the neural tube Arrest migration of trunk level neural crest cells near dorsal aorta Induce (i) migration of cells to form superior cervical ganglion, (ii) segmentation of cell columns into ganglia and (iii) axon outgrowth along blood vessels Essential for axon ingrowth into salivary glands, eye and spleen. Britsch et al. (1998) Kawasaki et al. (2002) Promote migration of neural crest cells to the correct site Promotes projection of axons from ciliary ganglion towards eye Enomoto et al. (2000) Hashino et al. (2001) 2.1.1. Netrins Netrins are a conserved family of secreted proteins (f 600 amino acids) that share some homology to laminin (see Dickson and Keleman, 2002). They have been shown to act as bifunctional neural guidance cues, exerting either attractive or repulsive effects. To date, four vertebrate members of the netrin family have been identified (netrins 1 –4). Netrins interact with two main families of receptors, UNC5 and DCC (deleted in colorectal cancer) families. The repulsive effects of netrin involve the UNC5 family of receptors, and the attractive effects of netrin are mediated through the DCC family of receptors, although the DCC family of receptors have also been implicated in repulsion. 2.1.2. Semaphorins Semaphorins are a conserved family of secreted and membrane-bound proteins (see Pasterkamp and Kolodkin, 2003) that are predominantly known for their role in neural repulsion. To date, more than 30 semaphorins have been identified. Semaphorins have been classified into eight groups on the basis of sequence similarity and distinctive structural features. They are typically around 750 amino acids in length and are defined by a conserved semaphorin domain ( f 500 amino acids) that contains 14 – 16 conserved cysteines, several blocks of conserved residues and no obvious repeat at their amino terminus. Two receptor families have been implicated in mediating semaphorin function, the plexins and neuropilins. Members of the GPI-linked and transmembrane classes of semaphorins bind directly to the plexin family of receptors. To date, at least nine plexins have been identified and classified into four subfamilies (plexins A –D) based on structural similarities. Enomoto et al. (2001); Honma et al. (2002) Glebova and Ginty (2004) Secreted semaphorins interact directly with the neuropilin family of receptors, which in turn form a receptor complex with the plexins. 2.1.3. Slits Slits are a family of large, secreted proteins containing four leucine-rich repeats surrounded by conserved N- and C-terminal domains, nine EGF-like repeats, an ALPS domain and a cysteine-rich carboxyl terminal domain (see Wong et al., 2002). Slits are primarily known for their role in neural repulsion. To date, three vertebrate members of the slit family have been identified. Slit-induced repulsion is mediated via a family of receptors called roundabout (Robo). Three vertebrate members of the robo family have been identified (robos 1– 3). 2.1.4. Ephrins Ephrins are a family of membrane-bound proteins (see Himanen and Nikolov, 2003) that are best known for their role in repulsion, although attractive effects have also been described. Ephrins are characterised by the presence of a unique N-terminal receptor-binding domain that is separated from the membrane via a linker of around 40 amino acids. To date, eight ephrins have been identified and are subdivided into two classes based on their structure and receptor binding preferences. EphrinAs (ephrinAs 1 –5) are anchored to the membrane via a GPI linkage and ephrinBs (ephrinBs 1– 3) have a transmembrane region and a short, but highly conserved cytoplasmic domain, which includes a PDZbinding motif. Ephrins interact with a family of receptors called Ephs. Eph receptors are transmembrane proteins that contain a highly conserved N-terminal domain followed by a H.M. Young et al. / Autonomic Neuroscience: Basic and Clinical 112 (2004) 1–14 cysteine-rich region and two fibronectin type III repeats in the extracellular domain, and a conserved kinase domain, a SAM domain and a PDZ-binding motif in the cytoplasmic region. To date, 14 members of the Eph family have been identified and classified into two subfamilies based on their sequence similarity and binding affinities for the ephrins. In general, the EphAs (EphAs 1 – 8) promiscuously interact with the GPI-linked ephrinAs, and the EphBs (EphBs 1 – 6) interact with the transmembrane ephrinBs. In addition to their promiscuity, the Ephs and ephrins are unique in the fact that they mediate bi-directional signalling, meaning that both the Eph and ephrin can serve as a receptor and as a ligand. 2.2. Neurotrophic factors Some molecules that are classified as neurotrophic factors because of their effects on neuronal survival can also regulate neural migration and the direction of axon outgrowth (Markus et al., 2002). For example, it was shown many years ago that the neurites of chick dorsal root ganglia grow towards a source of nerve growth factor (NGF) (Gundersen and Barrett, 1979) and that growth of sympathetic axons is induced by artificial sources of NGF in vivo (Levi-Montalcini and Angeletti, 1968). Members of the glial cell line-derived neurotrophic factor (GDNF) family have also been shown to influence neural migration and neurite outgrowth. As described in later sections of this article, GDNF, artemin and neurturin appear to be important guidance cues during the development of the enteric, sympathetic and parasympathetic nervous systems. GDNF family ligands signal through a receptor complex composed of a signaling sub-unit, Ret tyrosine kinase, that is common to all members of the GDNF family, and a binding sub-unit that is specific for each ligand (GFRa1 for GDNF, GFRa2 for neurturin and GFRa3 for artemin). 2.3. Extracellular matrix and cell adhesion molecules (CAMs) Extracellular matrix molecules form substrata along which neural cells migrate and axons grow. Migrating neural crest cells and neurites of developing autonomic neurons express a variety of extracellular matrix receptors. Some components of the extracellular matrix enhance or are permissive for neural migration and axon outgrowth (for example, laminin, collagen and fibronectin), whereas other molecules are usually inhibitory to migration and axon outgrowth (for example, chondroitin sulphate proteoglycan and tenascin). The role of the extracellular matrix in neural crest cell migration has been reviewed previously (Newgreen, 1992; Henderson and Copp, 1997; Perris, 1997), and is only summarized briefly in the current review. CAMs can also influence neural migration and axon outgrowth by mediating cell –cell and cell – substrate contacts. Different CAMs can show homophilic or heterophilic binding, or both. The role of CAMs in neural crest cell 3 migration has been reviewed previously (Newgreen and Tan, 1993) and, although there is little information available about the role of CAMs in autonomic axon growth, some CAMs have been shown to influence sympathetic axon growth (see Section 3.3). 3. Development of the enteric nervous system The vast majority of enteric neurons and glial cells arise from neural crest cells that emigrate from the post-otic hindbrain adjacent to somites 1– 7 (Yntema and Hammond, 1954; Le Douarin and Teillet, 1973). Vagal neural crest cells enter the foregut, and then migrate caudally within the gut wall to colonize the entire gut. Neural crest cells that emigrate from the sacral level of the neural axis also give rise to a small proportion of enteric neurons and glial cells, mostly in the large intestine (Burns and Le Douarin, 1998). 3.1. Migration of vagal level neural crest cells into and along the gut In addition to the enteric nervous system, vagal level neural crest cells give rise to other derivatives, including ganglia of the IXth and Xth cranial nerves, components of the cardiovascular system and contribute to the caudal branchial arches. It has been suggested that the differential expression of receptors by specific sub-populations of neural crest cells could determine their migration pathway by determining their response to localized ligands within the embryos (Wehrle-Haller and Weston, 1997). In zebrafish, some cranial neural crest cells appear to be specified prior to emigration from the neural tube (Schilling and Kimmel, 1994). It is unclear whether vagal neural crest cells are specified with an ability to enter the gut prior to emigration. Following transplantation of pre-migratory vagal neural crest cells from quail embryos to the trunk level of chick embryos, quail cells were reported in the gut of the chick host embryos (Le Douarin and Teillet, 1974). This suggests that vagal and trunk cells show different responses to the same environmental cues or have inherently different migratory abilities. In contrast, after performing similar experiments, Erickson and Goins (2000) reported that vagal cells transplanted to the thoracic region migrated only as far as the dorsal aorta, suggesting that the vagal cells are not specified prior to emigration. The mechanisms that guide only a sub-population of vagal level neural crest cells into the developing gut are unknown. In embryonic mice, Gdnf mRNA is expressed by the foregut mesenchyme prior to the entry of vagal neural crest cells (Natarajan et al., 2002). As vagal crest cells start to express Ret prior to their entry into the gut (Durbec et al., 1996), and as in vitro studies have shown that GDNF is chemoattractive to vagal crest cells prior to their entry into the gut, it is likely that GDNF plays a role in inducing vagal neural crest cells to enter the gut (Natarajan et al., 2002). 4 H.M. Young et al. / Autonomic Neuroscience: Basic and Clinical 112 (2004) 1–14 GDNF is also chemoattractive to neural crest-derived cells within the gut (Young et al., 2001; Natarajan et al., 2002; Iwashita et al., 2003), and thus GDNF produced by the gut mesenchyme probably plays a role in retaining neural crest cells within the gut so that they do not migrate into neighbouring tissues via the mesentery, or into pharyngeal or pelvic tissues (Young et al., 2001). GDNF may also play a direct role in the rostral-to-caudal migration of vagal neural crest cells along the gut. Natarajan et al. (2002) reported that there are high levels of Gdnf mRNA expression in the stomach and then later in the caecum, which precede the colonization of those regions by neural crest cells. In addition, neural crest cells may still migrate towards regions lacking other crest cells because of the presence of available (unbound) GDNF in the mesenchyme (Young et al., 2001). Vagal neural crest cell migration along the gut is also likely to be influenced by the composition of the extracellular matrix. A variety of extracellular matrix molecules, including fibronectin, laminin, J1/tenascin, and chondroitin sulphate proteoglycan are present within the embryonic gut wall during the time that vagal neural crest cells are colonizing the gut (Payette et al., 1988; Rothman et al., 1993, 1996; Newgreen and Hartley, 1995; Rauch and Schafer, 2003). Neural crest cells within the gut also express a range of receptors that recognize components of the extracellular matrix including laminin binding proteins (Chalazonitis et al., 1997; Howard and Gershon, 1998) and integrins (Kruger et al., 2002; Iwashita et al., 2003). In the embryonic rat gut, neural crest cells appear to migrate in a zone between high levels of inhibitory molecules— chondroitin sulphate proteoglycan close to the endoderm and J1/tenascin close to the serosa (Newgreen and Hartley, 1995). Molecules that promote neural crest cell migration, such as fibronectin and laminin, are widely distributed and have been proposed to play only a permissive role in the migratory route followed by neural crest cells as they colonize the gut (Newgreen and Hartley, 1995). Interestingly, in some mutant mice in which vagal neural crest cells fail to colonize the entire gastrointestinal tract, there are alterations in the expression of a number of extracellular matrix molecules in the mesenchyme of the aganglionic region (Payette et al., 1988; Tennyson et al., 1990; Rothman et al., 1996). However, it is unknown whether these are primary defects or secondary defects that occur due to an absence of enteric ganglia. 3.2. Migration of sacral level neural crest cells into the hindgut After emigrating from the neural tube, sacral neural crest cells migrate ventrally towards the distal hindgut. However, in both avian and mouse embryos, there appears to be a delay before sacral-derived cells enter the hindgut (Burns and Le Douarin, 1998; Burns et al., 2000; Kapur, 2000). In chick embryos, the sacral cells aggregate into the ganglia of the nerve of Remak (a chain of parasympathetic ganglia found in birds), and then 3– 4 days later, after the vagal neural crest cells have colonized the hindgut, a sub-population of cells migrate into the hindgut in close association with the axons of neurons in the nerve of Remak (Burns and Le Douarin, 1998). In embryonic mice, it appears that some of the sacral-derived crest cells that cluster close to the hindgut from embryonic day (E) 10.5 enter the distal gut after a delay of at least 4 days, while others give rise to neurons and glial cells of the pelvic plexus (Kapur, 2000; R.B.A., unpublished observation). It is unknown why there is an apparent delay in the entry of sacral neural crest cells into the hindgut. It is possible that there is (i) an early absence of attractive molecules in the hindgut (or their receptors on sacral crest cells) or (ii) a transient expression of inhibitory molecules in the hindgut. The secreted semaphorin, Sema3A, is transiently expressed in the distal hindgut of the embryonic chick and has been shown to be repulsive to the axons of neurons in the nearby nerve of Remak (Shepherd and Raper, 1999). The entry of the axons of neurons in the nerve of Remak into the hindgut coincides with the down-regulation of Sema3A by the outer mesenchyme (Shepherd and Raper, 1999). As sacral neural crest cells have been reported to migrate into the distal hindgut along the axons of neurons in the nerve of Remak (Burns and Le Douarin, 1998), it is possible that the expression of Sema3A also influences the migration of sacral neural crest cells into the gut and may be responsible for their delayed entry (Young and Newgreen, 2001; Newgreen and Young, 2002). Interestingly, when pre-migratory vagal neural crest cells are transplanted to the sacral level of the neural axis, they enter the hindgut without delay (Burns et al., 2002). These data indicate that the cue that delays the entry of sacral neural crest cells into the hindgut is not detected by vagal cells, and thus the signaling mechanisms controlling the entry of vagal and sacral neural crest cells into the avian hindgut are different. The studies described above, and studies in which neural crest-derived cells within the gut were localized using a variety of markers (Kapur et al., 1992; Young et al., 1998), suggest that there is a delay in the entry of sacral neural crest cells into the hindgut. However, there are also some studies that have reported an early arrival of sacral cells into the hindgut (Pomeranz and Gershon, 1990; Serbedzija et al., 1991; Erickson and Goins, 2000). Possible reasons for the discrepancy between the different studies have been discussed in detail previously (see Newgreen and Young, 2002), and include surgical artifacts and mis-identification of neural crest cells. In addition, Erickson and Goins (2000) have suggested that different groups may have examined different rostrocaudal levels of the hindgut; they observed an early arrival of sacral neural crest cells into the cloaca (the distal most part of the avian gut), but in slightly more rostral regions, they observed the same delay in entry reported by Burns and Le Douarin (1998). To date, there are no published reports on the expression of Sema3A in the cloacal wall. H.M. Young et al. / Autonomic Neuroscience: Basic and Clinical 112 (2004) 1–14 3.3. Centripetal migration of cells from the myenteric region to form the submucous plexus of the gut, and from the gut into the pancreas In most regions of the mature gastrointestinal tract, neurons are found in two ganglionated plexuses—an outer myenteric plexus between the circular and longitudinal muscle layers, and an inner submucosal plexus, at the inner margin of the circular muscle. In the small intestine, vagal neural crest cells migrate through the outer half of the mesenchyme and then settle just beneath the serosa, in the myenteric region (between where the longitudinal and circular muscle layers will form). The colonization of the submucosal region does not occur until several days later, probably from a secondary migration of cells from the myenteric region. In the hindgut, the migratory pathways taken by the vagal cells vary between species. In avian embryos, vagal cells migrate and settle first at the inner margin of the developing hindgut circular muscle layer, where the submucosal plexus will form (Burns and Le Douarin, 1998), whereas in embryonic mice, most vagal cells settle in the myenteric region, just under the serosa, and then a secondary migration to the submucosal region occurs later (McKeown et al., 2001). A recent study has shown that the centripetal migration of cells, from the myenteric to the submucosal region, is mediated by netrins and DCC (Jiang et al., 2003). In embryonic chicks and mice, the gut epithelium expresses netrins (netrins 1 and 3 in mice and netrin 2 in chick), and neural crest-derived cells within the gut express the netrin receptor, DCC (Seaman et al., 2001). In vitro assays showed that netrin is chemoattractive to enteric neural crest cells, and importantly, in mice lacking DCC, there are no submucosal ganglia (Jiang et al., 2003). Interestingly, although netrins are expressed by the epithelial cells, neural crest cells do not migrate into the mucosa, but form ganglia at the inner border of the circular muscle. Hence, there must be some, as yet unidentified, ‘‘stop’’ mechanism that prevents them from entering the mucosa, where the concentration of netrins would be highest. Neurons in the pancreas arise from cells that migrate out of the small intestine (Kirchgessner et al., 1992). Jiang et al. (2003) also showed that netrins are expressed by the pancreas, and that netrin-DCC signaling is required for the migration of cells into the pancreas. Mice lacking GFRa2, the ligand binding molecule for neurturin, also show a dramatic reduction in the number of pancreatic neurons, but it is unclear whether this is due to a failure of their precursors to migrate into the pancreas, or a requirement for neurturin signaling for survival and differentiation (Rossi et al., 2003). 3.4. Projection of axons by enteric neurons There are many different types of enteric neurons that differ in their axon projection patterns and target cells (Costa et al., 1996; Furness, 2000). For example, there are intrinsic 5 sensory neurons that project predominantly circumferentially around the gut, ascending and descending circular muscle motor neurons, longitudinal muscle motor neurons, secretomotor neurons, ascending interneurons and descending interneurons. Very little is known about the mechanisms controlling the axon projections of developing enteric neurons. Neurons begin to differentiate while vagal neural crest cells are migrating rostrocaudally along the gut, and many of the first axons project in the same direction (caudally or anally) and follow the same pathway through the mesenchyme as the migrating crest cells (Young et al., 1999, 2002). In a number of other locations including ventral roots and cranial nerves, neural crest cells are also closely associated with growing nerve fibres (Rickmann et al., 1985; Loring and Erickson, 1987; Noakes and Bennett, 1987; Carpenter and Hollyday, 1992; Noakes et al., 1993; Gilmour et al., 2002). In the lateral line nerve of the zebrafish, Gilmour et al. (2002) demonstrated that the growing axons were the source of cues that guided the neural crest cells, but in most instances, it is unclear whether both the neural crest cells and the axons are responding to the same (non-neural) environmental cue, or whether the axons or the neural crest cells are the source of a cue. In co-culture experiments in which vagal neural crest cells were forced to enter the distal hindgut and migrate rostrally (rather than caudally as they do normally), most of the neurons also projected rostrally (rather than caudally as they do normally), indicating that the direction of neural crest cell migration and axon projection are linked, and that the polarity of the gut itself is not an important influence on the axon projections of the first enteric neurons (Young et al., 2002). Many myenteric neurons have axons that project either orally (rostrally) or anally (caudally) to innervate the circular muscle. The orally projecting motor neurons are cholinergic and the anally projecting motor neurons use a combination of neurotransmitters including nitric oxide, ATP and vasoactive intestinal peptide (Costa et al., 1996; Sang and Young, 1996; Furness, 2000). It is unknown how a differentiating enteric neuron detects the polarity of the gut, and how the correlation between direction of axon projection and neurotransmitter type develops—whether neurons first become cholinergic and then project an axon orally, or whether orally projecting motor neurons become cholinergic neurons. Mice lacking neurturin (a member of the GDNF family) or GFRa2, which forms part of the receptor complex for neurturin, have a reduced number of cholinergic nerve fibres (detected by their content of substance P or by acetylcholinesterase staining) in the circular muscle, but no change in the number of nitric oxide-containing nerve fibres (Heuckeroth et al., 1999; Rossi et al., 1999, 2003). The number of myenteric neurons in the small intestine and colon of mice lacking neurturin is not significantly different from wildtype mice, and thus the deficits in the innervation of the circular muscle are not due to reduced myenteric neuron number (Gianino et al., 2003). As neurturin mRNA is expressed in the circular muscle layer and GFRa2 mRNA 6 H.M. Young et al. / Autonomic Neuroscience: Basic and Clinical 112 (2004) 1–14 is expressed in myenteric ganglia during both embryonic and post-natal development (Heuckeroth et al., 1999; Rossi et al., 1999; Dolatshad et al., 2002), neurturin could play role in inducing a sub-population of myenteric neurons to project an axon into the circular muscle layer and/or influence axon growth within the muscle. Studies in which explants of embryonic gut were grown in organ culture have shown that neurturin promotes neurite outgrowth (Taraviras et al., 1999; Yan et al., 2004). In vitro, GDNF also induces neurite outgrowth from embryonic and post-natal enteric neurons (Schafer and Mestres, 1999; Young et al., 2001; Natarajan et al., 2002), but its role in axon growth within the gut in vivo is unknown. that neural crest cell and motoneuron axon navigation through the somites is regulated by cues arising from the somites. The molecular basis of trunk neural crest cell migration through the rostral half of individual somites has been reviewed in detail recently (Krull, 2001; Halloran and Berndt, 2003), so we will only briefly review the subject in this article. A range of molecules are differentially expressed by the rostral and caudal halves of somites (Fig. 1A). In chick embryos, the caudal half of each somite expresses both Sema3A (Adams et al., 1996; Giger et al., 1996; Shepherd et al., 1996; Eickholt et al., 1999) and ephrin-B1 (Krull et al., 1997; Wang and Anderson, 1997; Koblar et al., 2000), and trunk neural crest cells express neuropilin-1 (Kawakami et al., 1996; Kawasaki et al., 2002) 4. Sympathetic nervous system The development of sympathetic neurons can be broken down into three major steps: (1) Neural crest cells from the trunk level of the neural axis delaminate from the dorsal regions of the neural folds and neural tube and migrate ventromedially through the rostral half of each somite. (2) After passing through the somites, neural crest cells migrate further ventrally and coalesce into ganglia adjacent to the dorsal aorta. (3) Molecules released by the dorsal aorta induce the cells to differentiate into neurons, which project axons to a variety of peripheral targets. 4.1. Emigration from the neural tube and migration ventromedially through the rostral half of each somite Two different pathways are followed by neural crest cells that emigrate from the trunk level of the neural axis; a ventromedial pathway and a dorsolateral pathway. The cells that follow a ventromedial pathway migrate through the rostral half of each somite and give rise to dorsal root and sympathetic ganglia. Cells following a dorsolateral pathway migrate under the ectoderm and give rise to melanocytes. Cells that follow a ventromedial pathway emigrate from the neural tube before those following a dorsolateral pathway (Serbedzija et al., 1989; Erickson et al., 1992), and it has been shown recently that ephrin-B ligands, produced by the dermomyotome, prevent the early emigrating cells from migrating into the dorsolateral path (Santiago and Erickson, 2002). Neural crest cells following the ventromedial pathway migrate through the rostral, but not caudal, half of each somite (Rickmann et al., 1985; Erickson et al., 1989), and axons of spinal motoneurons also project only through the rostral halves of the somites (Keynes and Stern, 1988). As a consequence, dorsal root ganglia and spinal nerves are segmental (Keynes and Stern, 1984). Microsurgical experiments in which the rostrocaudal polarity of individual somites was reversed (Keynes and Stern, 1984), or in which the caudal halves of individual somites were replaced with rostral halves (Kalcheim and Teillet, 1989), demonstrated Fig. 1. Diagrams showing the migratory pathways of trunk neural crest cells and the location of cues that influence their migratory behaviour. (A) Neural crest cells are channelled into the rostral half of each somite by a combination of repulsive cues in the caudal half of each somite including Ephrin-Bs, Sema3A and F-spondin. See Krull (2001) for review. (B) The migration of cells to form sympathetic ganglia is influenced by cues in the dermamyotome, and notochord (noto) and probably also by cues expressed by the tissue dorsal to the gut which prevent trunk neural crest cells from entering the gut. DRG—dorsal root ganglion; PNA-binding GCs—peanut agglutinin-binding glycoconjugates. H.M. Young et al. / Autonomic Neuroscience: Basic and Clinical 112 (2004) 1–14 and EphB3 (Krull et al., 1997), the receptors for Sema3A and ephrin-B1, respectively. Both Sema3A (Eickholt et al., 1999) and ephrin-B1 (Krull et al., 1997; Koblar et al., 2000) have been shown to be inhibitory to migrating trunk neural crest cells. Surprisingly, treatment of avian embryos with soluble ephrin-B1 perturbs the migration of neural crest cells, but not the outgrowth of axons of spinal motoneurons, indicating that different guidance cues may be used by axons and neural crest cells to avoid the caudal half of each somite (Koblar et al., 2000). Some extracellular matrix molecules that are inhibitory to migrating neural crest cells are also present in the caudal half of each somite and are likely to contribute to the exclusion of neural crest cells from the caudal halves of somites (see Krull, 2001). These include F-spondin (Debby-Brafman et al., 1999) and some chondroitin sulfate proteoglycans (see Krull, 2001). The expression of multiple repulsive cues by the caudal half of each somite raises the issue of the contribution of each guidance cue to migratory behaviour and whether there is functional redundancy. Perturbation of ephrin-B1 signalling in chick embryos is sufficient to perturb the segmental migration of neural crest cells through the somites, indicating that this signaling pathway is essential (Krull et al., 1997; Koblar et al., 2000). However, mice lacking ephrin-B2 (which may play a similar role in crest cell migration through the caudal half of each somite in rodents to that played by ephrin-B1 in chick embryos) have apparently normal patterns of neural crest cell migration through the somites (Wang et al., 1998). Similarly, mice lacking components of the Sema3A signaling pathway do not show any defects in their migration through the somites (Kawasaki et al., 2002). Thus, there appears to be redundancy in the mechanisms controlling crest cell migration through the somites in mice, which will only be confirmed by analysis of double knockouts. 4.2. Neural crest cells coalesce into ganglia adjacent to the dorsal aorta, and some undergo a secondary migration to form the superior cervical ganglion (SCG) Neuregulin signaling appears to be required for the migration of trunk neural crest cells ventral to the somites. The neuregulin-1 gene encodes a number of different isoforms of an EGF-like factor, whose effects are mediated by members of the ErbB family of receptor tyrosine kinases (Falls, 2003). Trunk neural crest cells express ErbB2 and ErbB3, and neuregulin-1 is expressed by newly formed somites, the mesenchyme surrounding the dorsal aorta and by the dorsal neural tube (Britsch et al., 1998). In mice lacking neuregulin-1, ErbB2 or ErbB3, neural crest cells delaminate from the neural tube normally and form dorsal root ganglia, but the cells that would normally migrate further ventrally to form the sympathetic ganglia remain in the dorsal half of the mutant embryos (Britsch et al., 1998). During the migration of sympathetic neuron precursors, neuregulin signaling is probably not acting as a directional guidance cue, but rather as a positive regulator of cells 7 motility. Thus, in the absence of neuregulin signaling, trunk neural crest cells appear to become immobile prematurely and accumulate dorsally, rather than migrating ventrally to form sympathetic ganglia (Britsch et al., 1998). Trunk neural crest cells that migrate ventrally, beyond the level of the neural tube and somites, coalesce into ganglia adjacent to the dorsal aorta (Fig. 1B). In mice lacking Sema3A or its receptor, neuropilin 1, many neural crest cells are dispersed and are present in abnormal locations both lateral (close to the forelimb buds) and medial (close to the midline) to the normal locations of sympathetic ganglia (Kawasaki et al., 2002). Sema3A is expressed in the dermamyotome and the forelimb bud in mice and chickens (Kawasaki et al., 2002), and also by the notochord in chickens (Anderson et al., 2003). Kawasaki et al. (2002) have proposed that Sema3A is a repulsive cue, and that the migration of neural crest cells is arrested when they are adjacent to the dorsal aorta because this location is at the bottom of a Sema3A gradient (Fig. 1B). It is important to note, however, that although many studies have demonstrated that a variety of members of the Sema3 sub-family are repulsive to the neurites of sympathetic neurons (Giger et al., 1998; Kawasaki et al., 2002; Atwal et al., 2003), only one study (Eickholt et al., 1999) has shown that Sema3A is also inhibitory to migratory neural crest cells. Recent studies have shown that the repulsive effects of the notochord on dorsal root ganglia and spinal motoneuron axons are mediated by Sema3A plus other unidentified repulsive signals (Anderson et al., 2003; Masuda et al., 2003), but it is unclear whether the repulsive effect of the notochord on migrating neural crest cells (Newgreen et al., 1986) is mediated by Sema3A only or by a combination of repulsive cues. The migration of neural crest cells through the rostral halves of the somites results in the dorsal root ganglia being segmental (Kalcheim and Teillet, 1989). Interestingly, however, when neural crest cells cease migrating and settle adjacent to the dorsal aorta, there is no obvious evidence of segmentation (Fig. 2). Hence, unlike dorsal root ganglia, the segmentation of sympathetic ganglia does not appear to be imposed by migration of neural crest cells through the rostral halves of the somites. Instead segmental sympathetic ganglia are likely to form by the rostral or caudal migration of cells within the cell columns. The SCG is thought to arise from cells that first migrate ventrally to coalesce into a column between cervical vertebrae C1 – C7, and then many of these cells migrate rostrally to separate from the stellate ganglion and form the SCG between C1 and C4 (Rubin, 1985; Nishino et al., 1999). The rostral migration of SCG precursors appears to involve a member of the GDNF family, artemin, acting at its receptor complex, Ret and GFRa3. In a large proportion of mice lacking artemin, Ret or GFRa3, the SCG is found caudal to its normal location (Durbec et al., 1996; Nishino et al., 1999; Enomoto et al., 2001; Honma et al., 2002). In these mutant mice, the ventral migration of SCG precursors appears to be 8 H.M. Young et al. / Autonomic Neuroscience: Basic and Clinical 112 (2004) 1–14 Fig. 2. Inverted fluorescence micrograph showing a lateral view of a wholemount preparation of the dorsal aorta with attached sympathetic neuron precursors on one side only from an E10.5 mouse. The sympathetic precursors were stained using an antibody to Phox2b. At the rostral end, cells are beginning to cluster into ganglia, but more caudally, discrete ganglia cannot be discerned. Scale bar: 100 Am. normal but their subsequent rostral migration is perturbed (Nishino et al., 1999; Enomoto et al., 2001). Sympathetic neuron precursors express Ret and GFRa3, and in vivo studies have shown that an artificial source of artemin induces migration of developing sympathetic neurons (Pachnis et al., 1993; Durbec et al., 1996; Nishino et al., 1999; Enomoto et al., 2001; Honma et al., 2002). Artemin is expressed both within the SCG and in the region surrounding the SCG, consistent with a role for artemin in the rostral migration of SCG precursors (Honma et al., 2002). Mice lacking GFRa3 and artemin also show segmentation defects in the more caudal sympathetic ganglia (Honma et al., 2002). In the thoracic and lumbar regions of embryonic mice, sympathetic chain ganglia form at locations where blood vessels, at each segment, branch off the dorsal aorta. As artemin is expressed by blood vessels (see Section 3.3), and artemin is chemoattractive to developing sympathetic neurons (Honma et al., 2002), artemin may play a role in the rostral or caudal migration of cells that lead to the segmentation of columns of cells into ganglia throughout the sympathetic chain. Trunk neural crest cells never migrate ventrally beyond the dorsal aorta into the gut (Le Douarin and Teillet, 1973, 1974). Two inhibitory or repulsive cues have been proposed to play a role in preventing trunk neural crest cells from entering the gut Slit – Robo signaling (De Bellard et al., 2003) and glycoconjugates that bind peanut agglutinin (de Freitas et al., 2003). In chick embryos, Slit1, -2 and -3 are expressed in the splanchnic mesoderm, dorsal to the gut, and trunk neural crest cells express Robo receptors (De Bellard et al., 2003; Fig. 1B). As Slit2 is repulsive to trunk neural crest cells, it has been suggested that Slit proteins play a role in preventing trunk neural crest cells from entering the gut (De Bellard et al., 2003). Interestingly, vagal neural crest cells do not express Robo receptors, and thus the colonization of the gut by vagal, but not trunk, neural crest cells has been attributed to the lack of expression of Robo receptors by vagal neural crest cells (De Bellard et al., 2003). Peanut agglutinin binding is transiently observed in tissue immediately dorsal to the gut at trunk, but not vagal or sacral levels of chick embryos (de Freitas et al., 2003). As peanut agglutinin binds to molecules that inhibit neural crest cell migration (Oakley and Tosney, 1991), it is possible that peanut agglutinin-binding molecules form a barrier that prevents neural crest cells from entering the gut at trunk, but not at vagal or sacral levels (de Freitas et al., 2003). 4.3. Developing sympathetic neurons project an axon to target tissues Neural crest cells that coalesce into ganglia adjacent to the dorsal aorta are induced to differentiate into sympathetic neurons by members of the bone morphogenetic protein (BMP) family, which are expressed by the dorsal aorta (Schneider et al., 1999). Shortly after the cells start to express catecholamine synthetic proteins and neuron-specific proteins, they extend an axon. Using a mutant strain of mice that lacks sweat glands, Guidry and Landis (1995) showed that the target tissue is not required to direct sympathetic axons to the vicinity of their targets. Thus, directional information must be provided along the pathway navigated by sympathetic axons. The axons of sympathetic neurons project in the grey rami, and then join the axons of sensory and motoneurons; these mixed peripheral nerves usually follow blood vessels to reach their targets. In mice lacking artemin, or its receptor components, Ret and GFRa3, many of the sympathetic axons fail to fasciculate into bundles as they exit the ganglia, and are stunted (Enomoto et al., 2001; Honma et al., 2002). Artemin is expressed by cells surrounding the developing sympathetic ganglia and also by the smooth muscle cells of blood vessels (Honma et al., 2002), and studies both in vivo and in vitro have shown that sympathetic axons grow preferentially towards an artifical source of artemin (Honma et al., 2002; Yan et al., 2003). Thus, artemin not only plays a role in the rostral migration of SCG precursors (see above), but it also appears to play a role in inducing sympathetic neurons to extend an axon and contributes to early sympathetic axon pathfinding by inducing them to grow along blood vessels. Interestingly, although the axons of sympathetic neurons run together with the axons of sensory and spinal motoneurons in peripheral nerves, artemin does not appear to influence the axon projections of sensory neurons (the projections of motoneurons was not examined) (Honma et al., 2002). Although there are little data available, it is likely that extracellular matrix and CAMs also stimulate sympathetic axon growth or direct growth along spatially restricted H.M. Young et al. / Autonomic Neuroscience: Basic and Clinical 112 (2004) 1–14 pathways. For example, the neural CAM, NrCAM, is a ligand for another CAM, axonin-1, and both have been localized within embryonic sympathetic ganglia (Lustig et al., 1999). A chimeric Fc-fusion protein of the extracellular region of Nr-CAM induces strong neurite outgrowth from sympathetic neurons from chick embryos which can be blocked by antibodies to axonin-1 (Lustig et al., 1999). Hence, interactions between Nr-CAM and axonin-1 could also promote neurite outgrowth from sympathetic neurons. Once they are in the vicinity of the target tissue, neurotrophic factors, produced by the target tissue, may induce sympathetic axons expressing the appropriate receptors to enter particular targets. As most tissues that are innervated by sympathetic axons express NGF, and as sympathetic axons grow towards a source of NGF (Levi-Montalcini and Angeletti, 1968), NGF is likely to play a role in inducing axons to enter particular tissues and inducing branching within target tissues, as well as providing trophic support. However, it has been difficult to distinguish between trophic and guidance roles for NGF. The exact effect of NGF on axon outgrowth and target innervation has been examined recently by generating mice deficient for both NGF and Bax (Glebova and Ginty, 2004). Bax is a pro-apoptotic gene and its absence prevents the death of neurons usually seen in NGF knockout animals. While sympathetic neuron numbers were normal and initial axon pathfinding largely unaffected, analysis of NGF / ; Bax / knockouts revealed that sympathetic axon growth into specific target organs was affected in different ways. Some target organs lacked a sympathetic innervation altogether (salivary glands and eye) while others were unaffected (trachea). However, the majority of organs showed a reduced sympathetic innervation. The spleen showed a striking phenotype, in that the ingrowing sympathetic axons grew along the lienal artery, but stalled at the boundary of the spleen, suggesting that, in this case, the requirement for NGF was focused at this boundary. The study confirms that, in addition to neuronal survival, NGF plays role in the growth of sympathetic axons into particular targets. However, the partial innervation of many organs in the absence of NGF confirms that successful sympathetic axon growth into peripheral targets is likely to depend on a range of factors with overlapping roles. The entry of sympathetic axons into some target tissues appears to be controlled by the neurotrophin, NT-3. In NT-3 / mice, sympathetic axons fail to enter the pineal gland and the external ear; infusion of exogenous NT-3 into the external ear restores the sympathetic innervation in the mutant mice (ElShamy et al., 1996). Interestingly, in NT-3 / mice, the sympathetic innervation of many target tissues is normal, demonstrating that not all sympathetic neurons have a requirement for NT-3 (ElShamy et al., 1996). GDNF is also expressed by a number of targets that are innervated by sympathetic neurons (Henderson et al., 1994; Trupp et al., 1995, 1996, 1997; Hellmich et al., 1996; Nosrat et al., 1997; Golden et al., 1999). As neurites from SCG and 9 lumbar sympathetic ganglia grow preferentially towards a source of GDNF in vitro (Yan et al., 2003), the presence of GDNF in some target tissues may also contribute to inducing sympathetic axons to enter particular targets. Extracellular matrix molecules and cell surface ligands expressed by target tissues may also be involved in the entry of sympathetic axons into particular targets. The myocardium of the developing heart expresses vascular cell adhesion molecule-1 (VCAM-1), which binds to a4h1 integrin (Wingerd et al., 2002). Sympathetic axons that innervate the developing heart express a4-integrins, and as function blocking antibodies to VCAM-1 or a4-integrin significantly reduce the sympathetic innervation of the heart, interactions between VCAM-1 and a4-integrins appear to be required for the entry of sympathetic axons into the heart (Wingerd et al., 2002). 5. Parasympathetic nervous system 5.1. Cranial parasympathetic ganglia Analysis of knockout mice lacking molecules required for GDNF or neurturin signaling has revealed heterogeneity amongst cranial parasympathetic ganglia in their requirements of GDNF family members—for example, the sphenopalatine ganglion appears to require GDNF and not neurturin whereas the otic ganglion requires both GDNF and neurturin (Enomoto et al., 2000; Rossi et al., 2000). However, in only a few instances are the precise roles of GDNF and neurturin known. Otic ganglion precursors express both components of the GDNF receptor, Ret and GFRa1, and GDNF is expressed in a gradient along the route that these precursors migrate (Enomoto et al., 2000). In mice lacking GDNF, the precursors do not follow the normal migratory pathway, and thus GDNF appears to act as a guidance cue for the migration of neural crest cells to the site where the otic ganglion will form (Enomoto et al., 2000). In the eye, both GDNF and neurturin are expressed by the ciliary muscle and striated muscle as the axons of ciliary neurons are growing towards these targets, and both GDNF and neurturin promote neurite outgrowth from ciliary ganglion neurons in vitro (Hashino et al., 2001). In chick embryos into which a GDNF function blocking antibody had been injected before the ciliary neurons projected an axon, very few ciliary neurons extended towards the eye (Hashino et al., 2001). Hence, GDNF and neurturin probably play a role in promoting the growth of the axons of ciliary neurons towards their targets. The sublingual and lacrimal glands of Gfra2 / mice lack parasympathetic nerve fibres, but the sympathetic innervation is unaffected (Rossi et al., 2000). Since a deficit in the parasympathetic innervation of the sublingual gland is already evident at birth, neurturin signaling may also be required for the growth of axons into this target. 10 H.M. Young et al. / Autonomic Neuroscience: Basic and Clinical 112 (2004) 1–14 5.2. Cardiac neural crest cells Some of the neural crest cells that emigrate from the neural tube adjacent to somites 1– 3 migrate to the developing heart. These cardiac neural crest cells not only give rise to the cardiac ganglia, but they also contribute to the outflow tracts and aortic arches (Creazzo et al., 1998). The migration of neural crest cells into the heart appears to involve the secreted semaphorin, Sema3C (Brown et al., 2001; Feiner et al., 2001). Sema3C is expressed in the myocardium of the outflow tract, and Sema3C / mice die at birth due to defects in the aortic arch and cardiac outflow tracts caused by a failure of cardiac neural crest cells to migrate to the correct locations (Feiner et al., 2001). As semaphorins are best known as repulsive cues, it is interesting that Sema3C may be acting as a chemoattractant to migrating cardiac neural crest cells. It is unclear whether members of the GDNF family are involved as guidance cues during development of cardiac ganglia. Late embryonic Ret / mice have a reduced number of neurons in the cardiac ganglia, but it is not know whether this is caused by a defect in neural crest cell migration, reduced proliferation or a decrease in survival (Hiltunen et al., 2000). Furthermore, adult mice lacking GFRa2 have a reduced density of cholinergic nerve fibres in the ventricles and ventricular conducting system (Hiltunen et al., 2000). However, it was not reported whether there is a change in the number of cardiac neurons in these mice, so it is unclear whether signaling via GFRa2 (presumably through neurturin) plays a role in neural crest cell migration, survival or proliferation, or inducing the axons of the cardiac neurons to enter the ventricles. 5.3. Parasympathetic ganglia in the airways Parasympathetic neurons associated with the airways probably arise from neural crest cells that migrate from the foregut into the lung buds or from neural crest cells that migrate into the lung along the vagus nerve (Tollet et al., 2001). GDNF is expressed by the developing lung (Towers et al., 1998), and in vitro studies have shown that GDNF is chemoattractive to neural crest-derived cells within the lung and influences the direction of neurite extension (Tollet et al., 2002). However, the role of GDNF in vivo in neural crest cell migration into the lung and axon extension is not known. 5.4. Pelvic neurons Neurons in pelvic ganglia include both sympathetic and parasympathetic neurons. Little is known about the development of pelvic neurons, although they are thought to arise from the sacral neural crest. Mice lacking GFRa2 have a reduced number of nitric oxide synthase-containing nerve fibres in the penis, but a normal number of sympathetic nerve fibres (Laurikainen et al., 2000a), but it is unknown whether this is due to a reduced number of parasympathetic neurons in the pelvic ganglia, reduced numbers of axons reaching their target, reduced branching or reduced survival (Laurikainen et al., 2000a,b). GDNF is also expressed by some targets innervated by pelvic neurons (Laurikainen et al., 2000b), but its role is unknown. 6. Conclusions During the assembly of the peripheral autonomic nervous system, migrating neural crest cells and outgrowing axons must navigate with precision to their targets. Although some of the inhibitory and attractive cues and substrates that enable migrating neural crest cells and the growth cones of autonomic neurons to navigate to the correct target have been identified, many remain to be identified. GDNF family members appear to play a more prominent role in neural navigation during the development of the autonomic nervous system than they do in other parts of the nervous system. Recent analysis of mice with null mutations in both Bax and NGF have revealed that NGF also plays a role in guiding axons into particular targets, as well as its well known trophic role for sympathetic neurons. Mice lacking individual components of the major neural guidance cue signaling pathways (semaphorin, slit, ephrin and netrin families) only rarely have shown defects in the peripheral autonomic nervous system. This suggests either that novel guidance cues are important or that there is considerable redundancy. The extent of this redundancy should be revealed in the future by analysis of double-knockout mice, or by using electroporation to interfere with multiple pathways in avian embryos. There are many outstanding questions to be resolved about the identification and role of neural guidance cues during the development of all of the major sub-divisions of the autonomic nervous system. During the development of the enteric nervous system, it is unknown how different classes of developing neurons (that project in different directions) ‘‘sense’’ the polarity of the gut. It is difficult to imagine a gradient of a single molecule operating along the entire gut or even along a single gut region (e.g., small intestine). Sympathetic neurons projecting to different targets differ in their phenotype; it is still unclear whether developing sympathetic neurons project randomly to different targets and the phenotype is determined solely by the target, or whether there is some specification prior to target contact so that specific subpopulations of neurons project their axons along different routes (because of different responses to localized ligands). Finally, currently very little is known about the development of parasympathetic neurons in general, apart from some cranial ganglia. The mechanisms by which neural crest cells navigate to particular organs and form ganglia are largely unknown. H.M. Young et al. / Autonomic Neuroscience: Basic and Clinical 112 (2004) 1–14 Acknowledgements The authors’ work is supported by the Australian Research Council (DP0345298 and DP0452272) and the National Health and Medical Research Council of Australia (project grant 145628 to HMY, Senior Research Fellowship 170224 to HMY and C.J. Martin Fellowship 007144 to RBA). References Adams, R.H., Betz, H., Puschel, A.W., 1996. A novel class of murine semaphorins with homology to thrombospondin is differentially expressed during early embryogenesis. Mech. Dev. 57, 33 – 45. Anderson, C.N., Ohta, K., Quick, M.M., Fleming, A., Keynes, R., Tannahill, D., 2003. Molecular analysis of axon repulsion by the notochord. Development 130, 1123 – 1133. Atwal, J.K., Singh, K.K., Tessier-Lavigne, M., Miller, F.D., Kaplan, D.R., 2003. Semaphorin 3F antagonizes neurotrophin-induced phosphatidylinositol 3-kinase and mitogen-activated protein kinase kinase signaling: a mechanism for growth cone collapse. J. Neurosci. 23, 7602 – 7609. Britsch, S., Li, L., Kirchhoff, S., Theuring, F., Brinkmann, V., Birchmeier, C., Riethmacher, D., 1998. The ErbB2 and ErbB3 receptors and their ligand, neuregulin-1, are essential for development of the sympathetic nervous system. Genes Dev. 12, 1825 – 1836. Brown, C.B., Feiner, L., Lu, M.M., Li, J., Ma, X., Webber, A.L., Jia, L., Raper, J.A., Epstein, J.A., 2001. PlexinA2 and semaphorin signaling during cardiac neural crest development. Development 128, 3071 – 3080. Burns, A.J., Le Douarin, N.M., 1998. The sacral neural crest contributes neurons and glia to the post-umbilical gut: spatiotemporal analysis of the development of the enteric nervous system. Development 125, 4335 – 4347. Burns, A.J., Champeval, D., Le Douarin, N.M., 2000. Sacral neural crest cells colonise aganglionic hindgut in vivo but fail to compensate for lack of enteric ganglia. Dev. Biol. 219, 30 – 43. Burns, A.J., Delalande, J.M., Le Douarin, N.M., 2002. In ovo transplantation of enteric nervous system precursors from vagal to sacral neural crest results in extensive hindgut colonisation. Development 129, 2785 – 2796. Carpenter, E.M., Hollyday, M., 1992. The distribution of neural crestderived Schwann cells from subsets of brachial spinal segments into the peripheral nerves innervating the chick forelimb. Dev. Biol. 150, 160 – 170. Chalazonitis, A., Tennyson, V.M., Kibbey, M.C., Rothman, T.P., Gershon, M.D., 1997. The alpha1 subunit of laminin-1 promotes the development of neurons by interacting with LBP110 expressed by neural crest-derived cells immunoselected from the fetal mouse gut. J. Neurobiol. 33, 118 – 138. Costa, M., Brookes, S.J., Steele, P.A., Gibbins, I., Burcher, E., Kandiah, C.J., 1996. Neurochemical classification of myenteric neurons in the guinea-pig ileum. Neuroscience 75, 949 – 967. Creazzo, T.L., Godt, R.E., Leatherbury, L., Conway, S.J., Kirby, M.L., 1998. Role of cardiac neural crest cells in cardiovascular development. Annu. Rev. Physiol. 60, 267 – 286. De Bellard, M.E., Rao, Y., Bronner-Fraser, M., 2003. Dual function of Slit2 in repulsion and enhanced migration of trunk, but not vagal, neural crest cells. J. Cell Biol. 162, 269 – 279. de Freitas, P.F., Ferreira Fde, F., Faraco, C.D., 2003. PNA-positive glycoconjugates are negatively correlated with the access of neural crest cells to the gut in chicken embryos. Anat. Rec. 273A, 705 – 713. Debby-Brafman, A., Burstyn-Cohen, T., Klar, A., Kalcheim, C., 1999. F-Spondin, expressed in somite regions avoided by neural crest cells, mediates inhibition of distinct somite domains to neural crest migration. Neuron 22, 475 – 488. 11 Dickson, B.J., Keleman, K., 2002. Netrins. Curr. Biol. 12, R154 – R155. Dolatshad, N.F., Silva, A.T., Saffrey, M.J., 2002. Identification of GFR alpha-2 isoforms in myenteric plexus of postnatal and adult rat intestine. Brain Res., Mol. Brain Res. 107, 32 – 38. Durbec, P.L., Larsson-Blomberg, L.B., Schuchardt, A., Costantini, F., Pachnis, V., 1996. Common origin and developmental dependence on c-ret of subsets of enteric and sympathetic neuroblasts. Development 122, 349 – 358. Eickholt, B.J., Mackenzie, S.L., Graham, A., Walsh, F.S., Doherty, P., 1999. Evidence for collapsin-1 functioning in the control of neural crest migration in both trunk and hindbrain regions. Development 126, 2181 – 2189. ElShamy, W.M., Linnarsson, S., Lee, K.F., Jaenisch, R., Ernfors, P., 1996. Prenatal and postnatal requirements of NT-3 for sympathetic neuroblast survival and innervation of specific targets. Development 122, 491 – 500. Enomoto, H., Heuckeroth, R.O., Golden, J.P., Johnson, E.M., Milbrandt, J., 2000. Development of cranial parasympathetic ganglia requires sequential actions of GDNF and neurturin. Development 127, 4877 – 4889. Enomoto, H., Crawford, P.A., Gorodinsky, A., Heuckeroth, R.O., Johnson Jr., E.M., Milbrandt, J., 2001. RET signaling is essential for migration, axonal growth and axon guidance of developing sympathetic neurons. Development 128, 3963 – 3974. Erickson, C.A., Goins, T.L., 2000. Sacral neural crest cell migration to the gut is dependent upon the migratory environment and not cell-autonomous migratory properties. Dev. Biol. 219, 79 – 97. Erickson, C.A., Loring, J.F., Lester, S.M., 1989. Migratory pathways of HNK-1-immunoreactive neural crest cells in the rat embryo. Dev. Biol. 134, 112 – 118. Erickson, C.A., Duong, T.D., Tosney, K.W., 1992. Descriptive and experimental analysis of the dispersion of neural crest cells along the dorsolateral path and their entry into ectoderm in the chick embryo. Dev. Biol. 151, 251 – 272. Falls, D.L., 2003. Neuregulins: functions, forms, and signaling strategies. Exp. Cell Res. 284, 14 – 30. Feiner, L., Webber, A.L., Brown, C.B., Lu, M.M., Jia, L., Feinstein, P., Mombaerts, P., Epstein, J.A., Raper, J.A., 2001. Targeted disruption of semaphorin 3C leads to persistent truncus arteriosus and aortic arch interruption. Development 128, 3061 – 3070. Furness, J.B., 2000. Types of neurons in the enteric nervous system. J. Auton. Nerv. Syst. 81, 87 – 96. Gianino, S., Grider, J.R., Cresswell, J., Enomoto, H., Heuckeroth, R.O., 2003. GDNF availability determines enteric neuron number by controlling precursor proliferation. Development 130, 2187 – 2198. Giger, R.J., Wolfer, D.P., De Wit, G.M., Verhaagen, J., 1996. Anatomy of rat semaphorin III/collapsin-1 mRNA expression and relationship to developing nerve tracts during neuroembryogenesis. J. Comp. Neurol. 375, 378 – 392. Giger, R.J., Urquhart, E.R., Gillespie, S.K., Levengood, D.V., Ginty, D.D., Kolodkin, A.L., 1998. Neuropilin-2 is a receptor for semaphorin: IV. Insight into the structural basis of receptor function and specificity. Neuron 21, 1079 – 1092. Gilmour, D.T., Maischein, H.M., Nusslein-Volhard, C., 2002. Migration and function of a glial subtype in the vertebrate peripheral nervous system. Neuron 34, 577 – 588. Glebova, N.O., Ginty, D.D., 2004. Heterogenous requirement of NGF for sympathetic target innervation in vivo. J. Neurosci. 24, 743 – 751. Golden, J.P., DeMaro, J.A., Osborne, P.A., Milbrandt, J., Johnson Jr., E.M., 1999. Expression of neurturin, GDNF, and GDNF family-receptor mRNA in the developing and mature mouse. Exp. Neurol. 158, 504 – 528. Guidry, G., Landis, S.C., 1995. Sympathetic axons pathfind successfully in the absence of target. J. Neurosci. 15, 7565 – 7574. Gundersen, R.W., Barrett, J.N., 1979. Neuronal chemotaxis: chick dorsalroot axons turn toward high concentrations of nerve growth factor. Science 206, 1079 – 1080. Halloran, M.C., Berndt, J.D., 2003. Current progress in neural crest cell 12 H.M. Young et al. / Autonomic Neuroscience: Basic and Clinical 112 (2004) 1–14 motility and migration and future prospects for the zebrafish model system. Dev. Dyn. 228, 497 – 513. Hashino, E., Shero, M., Junghans, D., Rohrer, H., Milbrandt, J., Johnson Jr., E.M., 2001. GDNF and neurturin are target-derived factors essential for cranial parasympathetic neuron development. Development 128, 3773 – 3782. Hellmich, H.L., Kos, L., Cho, E.S., Mahon, K.A., Zimmer, A., 1996. Embryonic expression of glial cell-line derived neurotrophic factor (GDNF) suggests multiple developmental roles in neural differentiation and epithelial – mesenchymal interactions. Mech. Dev. 54, 95 – 105. Henderson, D.J., Copp, A.J., 1997. Role of the extracellular matrix in neural crest cell migration. J. Anat. 191 (Pt 4), 507 – 515. Henderson, C.E., Phillips, H.S., Pollock, R.A., Davies, A.M., Lemeulle, C., Armanini, M., Simmons, L., Moffet, B., Vandlen, R.A., Simpson, L.C., et al., 1994. GDNF: a potent survival factor for motoneurons present in peripheral nerve and muscle. Science 266, 1062 – 1064. Heuckeroth, R.O., Enomoto, H., Grider, J.R., Golden, J.P., Hanke, J.A., Jackman, A., Molliver, D.C., Bardgett, M.E., Snider, W.D., Johnson Jr., E.M., Milbrandt, J., 1999. Gene targeting reveals a critical role for neurturin in the development and maintenance of enteric, sensory, and parasympathetic neurons. Neuron 22, 253 – 263. Hiltunen, J.O., Laurikainen, A., Airaksinen, M.S., Saarma, M., 2000. GDNF family receptors in the embryonic and postnatal rat heart and reduced cholinergic innervation in mice hearts lacking ret or GFRalpha2. Dev. Dyn. 219, 28 – 39. Himanen, J.P., Nikolov, D.B., 2003. Eph signaling: a structural view. Trends Neurosci. 26, 46 – 51. Honma, Y., Araki, T., Gianino, S., Bruce, A., Heuckeroth, R., Johnson, E., Milbrandt, J., 2002. Artemin is a vascular-derived neurotropic factor for developing sympathetic neurons. Neuron 35, 267 – 282. Howard, M.J., Gershon, M.D., 1998. Development of LBP110 expression by neural crest-derived enteric precursors: migration and differentiation potential in ls/ls mutant mice. J. Neurobiol. 35, 341 – 354. Iwashita, T., Kruger, G.M., Pardal, R., Kiel, M.J., Morrison, S.J., 2003. Hirschsprung disease is linked to defects in neural crest stem cell function. Science 301, 972 – 976. Jiang, Y., Liu, M.T., Gershon, M.D., 2003. Netrins and DCC in the guidance of migrating neural crest-derived cells in the developing bowel and pancreas. Dev. Biol. 258, 364 – 384. Kalcheim, C., Teillet, M.A., 1989. Consequences of somite manipulation on the pattern of dorsal root ganglion development. Development 106, 85 – 93. Kapur, R.P., 2000. Colonization of the murine hindgut by sacral crestderived neural precursors: experimental support for an evolutionarily conserved model. Dev. Biol. 227, 146 – 155. Kapur, R.P., Yost, C., Palmiter, R.D., 1992. A transgenic model for studying development of the enteric nervous system in normal and aganglionic mice. Development 116, 167 – 175. Kawakami, A., Kitsukawa, T., Takagi, S., Fujisawa, H., 1996. Developmentally regulated expression of a cell surface protein, neuropilin, in the mouse nervous system. J. Neurobiol. 29, 1 – 17. Kawasaki, T., Bekku, Y., Suto, F., Kitsukawa, T., Taniguchi, M., Nagatsu, I., Nagatsu, T., Itoh, K., Yagi, T., Fujisawa, H., 2002. Requirement of neuropilin 1-mediated Sema3A signals in patterning of the sympathetic nervous system. Development 129, 671 – 680. Keynes, R.J., Stern, C.D., 1984. Segmentation in the vertebrate nervous system. Nature 310, 786 – 789. Keynes, R.J., Stern, C.D., 1988. Mechanisms of vertebrate segmentation. Development 103, 413 – 429. Kirchgessner, A.L., Adlersberg, M.A., Gershon, M.D., 1992. Colonization of the developing pancreas by neural precursors from the bowel. Dev. Dyn. 194, 142 – 154. Koblar, S.A., Krull, C.E., Pasquale, E.B., McLennan, R., Peale, F.D., Cerretti, D.P., Bothwell, M., 2000. Spinal motor axons and neural crest cells use different molecular guides for segmental migration through the rostral half-somite. J. Neurobiol. 42, 437 – 447. Kruger, G., Mosher, J., Bixby, S., Joseph, N., Iwashita, T., Morrison, S., 2002. Neural crest stem cells persist in the adult gut but undergo changes in self-renewal, neuronal subtype potential, and factor responsiveness. Neuron 35, 657. Krull, C.E., 2001. Segmental organization of neural crest migration. Mech. Dev. 105, 37 – 45. Krull, C.E., Lansford, R., Gale, N.W., Collazo, A., Marcelle, C., Yancopoulos, G.D., Fraser, S.E., Bronner-Fraser, M., 1997. Interactions of Eph-related receptors and ligands confer rostrocaudal pattern to trunk neural crest migration. Curr. Biol. 7, 571 – 580. Laurikainen, A., Hiltunen, J.O., Thomas-Crusells, J., Vanhatalo, S., Arumae, U., Airaksinen, M.S., Klinge, E., Saarma, M., 2000a. Neurturin is a neurotrophic factor for penile parasympathetic neurons in adult rat. J. Neurobiol. 43, 198 – 205. Laurikainen, A., Hiltunen, J.O., Vanhatalo, S., Klinge, E., Saarma, M., 2000b. Glial cell line-derived neurotrophic factor is expressed in penis of adult rat and retrogradely transported in penile parasympathetic and sensory nerves. Cell Tissue Res. 302, 321 – 329. Le Douarin, N.M., Teillet, M.A., 1973. The migration of neural crest cells to the wall of the digestive tract in avian embryo. J. Embryol. Exp. Morphol. 30, 31 – 48. Le Douarin, N.M., Teillet, M.A., 1974. Experimental analysis of the migration and differentiation of neuroblasts of the autonomic nervous system and of neurectodermal mesenchymal derivatives, using a biological cell marking technique. Dev. Biol. 41, 162 – 184. Levi-Montalcini, R., Angeletti, P.U., 1968. Nerve growth factor. Physiol. Rev. 48, 534 – 569. Loring, J.F., Erickson, C.A., 1987. Neural crest cell migratory pathways in the trunk of the chick embryo. Dev. Biol. 121, 220 – 236. Lustig, M., Sakurai, T., Grumet, M., 1999. Nr-CAM promotes neurite outgrowth from peripheral ganglia by a mechanism involving axonin1 as a neuronal receptor. Dev. Biol. 209, 340 – 351. Markus, A., Patel, T.D., Snider, W.D., 2002. Neurotrophic factors and axonal growth. Curr. Opin. Neurobiol. 12, 523 – 531. Masuda, T., Tsuji, H., Taniguchi, M., Yagi, T., Tessier-Lavigne, M., Fujisawa, H., Okado, N., Shiga, T., 2003. Differential non-target-derived repulsive signals play a critical role in shaping initial axonal growth of dorsal root ganglion neurons. Dev. Biol. 254, 289 – 302. McKeown, S.J., Chow, C.W., Young, H.M., 2001. Development of the submucous plexus in the large intestine of the mouse. Cell Tissue Res. 303, 301 – 305. Natarajan, D., Marcos-Gutierrez, C., Pachnis, V., de Graaff, E., 2002. Requirement of signalling by receptor tyrosine kinase RET for the directed migration of enteric nervous system progenitor cells during mammalian embryogenesis. Development 129, 5151 – 5160. Newgreen, D.F., 1992. Establishment of the form of the peripheral nervous system. In: Hendry, I.A., Hill, C.E. (Eds.), Development, Regeneration and Plasticity of the Autonomic Nervous System. Harwood Academic, Switzerland, pp. 1 – 94. Newgreen, D.F., Hartley, L., 1995. Extracellular matrix and adhesive molecules in the early development of the gut and its innervation in normal and spotting lethal rat embryos. Acta Anat. (Basel) 154, 243 – 260. Newgreen, D.F., Tan, S.S., 1993. Adhesion molecules in neural crest development. Pharmacol. Ther. 60, 517 – 537. Newgreen, D., Young, H.M., 2002. Enteric nervous system: development and developmental disturbances—part 2. Pediatr. Dev. Pathol. 5, 329 – 349. Newgreen, D.F., Scheel, M., Kastner, V., 1986. Morphogenesis of sclerotome and neural crest in avian embryos. In vivo and in vitro studies on the role of notochordal extracellular material. Cell Tissue Res. 244, 299 – 313. Nishino, J., Mochida, K., Ohfuji, Y., Shimazaki, T., Meno, C., Ohishi, S., Matsuda, Y., Fujii, H., Saijoh, Y., Hamada, H., 1999. GFR alpha3, a component of the artemin receptor, is required for migration and survival of the superior cervical ganglion. Neuron 23, 725 – 736. Noakes, P.G., Bennett, M.R., 1987. Growth of axons into developing muscles of the chick forelimb is preceded by cells that stain with Schwann cell antibodies. J. Comp. Neurol. 259, 330 – 347. H.M. Young et al. / Autonomic Neuroscience: Basic and Clinical 112 (2004) 1–14 Noakes, P.G., Hornbruch, A., Wolpert, L., 1993. The relationship between migrating neural crest cells and growing limb nerves in the developing chick forelimb. In: Fallon, J.F., Goetinck, P.F., Kelly, R.O., Stocum, D.L. (Eds.), Limb Development and Regeneration. Part A. Progress in Clinical and Biological Research, vol. 383A. Wiley-Liss, New York, pp. 381 – 390. Nosrat, C.A., Tomac, A., Hoffer, B.J., Olson, L., 1997. Cellular and developmental patterns of expression of Ret and glial cell line-derived neurotrophic factor receptor alpha mRNAs. Exp. Brain Res. 115, 410 – 422. Oakley, R.A., Tosney, K.W., 1991. Peanut agglutinin and chondroitin-6sulfate are molecular markers for tissues that act as barriers to axon advance in the avian embryo. Dev. Biol. 147, 187 – 206. Pachnis, V., Mankoo, B., Costantini, F., 1993. Expression of the c-ret proto-oncogene during mouse embryogenesis. Development 119, 1005 – 1017. Pasterkamp, R.J., Kolodkin, A.L., 2003. Semaphorin junction: making tracks toward neural connectivity. Curr. Opin. Neurobiol. 13, 79 – 89. Payette, R.F., Tennyson, V.M., Pomeranz, H.D., Pham, T.D., Rothman, T.P., Gershon, M.D., 1988. Accumulation of components of basal laminae: association with the failure of neural crest cells to colonize the presumptive aganglionic bowel of ls/ls mutant mice. Dev. Biol. 125, 341 – 360. Perris, R., 1997. The extracellular matrix in neural crest-cell migration. Trends Neurosci. 20, 23 – 31. Pomeranz, H.D., Gershon, M.D., 1990. Colonization of the avian hindgut by cells derived from the sacral neural crest. Dev. Biol. 137, 378 – 394. Rauch, U., Schafer, K.H., 2003. The extracellular matrix and its role in cell migration and development of the enteric nervous system. Eur. J. Pediatr. Surg. 13, 158 – 162. Rickmann, M., Fawcett, J.W., Keynes, R.J., 1985. The migration of neural crest cells and the growth of motor axons through the rostral half of the chick somite. J. Embryol. Exp. Morphol. 90, 437 – 455. Rossi, J., Luukko, K., Poteryaev, D., Laurikainen, A., Sun, Y.F., Laakso, T., Eerikainen, S., Tuominen, R., Lakso, M., Rauvala, H., Arumae, U., Pasternack, M., Saarma, M., Airaksinen, M.S., 1999. Retarded growth and deficits in the enteric and parasympathetic nervous system in mice lacking GFR alpha2, a functional neurturin receptor. Neuron 22, 243 – 252. Rossi, J., Tomac, A., Saarma, M., Airaksinen, M.S., 2000. Distinct roles for GFRalpha1 and GFRalpha2 signalling in different cranial parasympathetic ganglia in vivo. Eur. J. Neurosci. 12, 3944 – 3952. Rossi, J., Herzig, K.H., Voikar, V., Hiltunen, P.H., Segerstrale, M., Airaksinen, M.S., 2003. Alimentary tract innervation deficits and dysfunction in mice lacking GDNF family receptor alpha2. J. Clin. Invest. 112, 707 – 716. Rothman, T.P., Chen, J., Howard, M.J., Costantini, F., Schuchardt, A., Pachnis, V., Gershon, M.D., 1996. Increased expression of laminin-1 and collagen (IV) subunits in the aganglionic bowel of ls/ls, but not c-ret / mice. Dev. Biol. 178, 498 – 513. Rothman, T.P., Le Douarin, N.M., Fontaine-Perus, J.C., Gershon, M.D., 1993. Colonization of the bowel by neural crest-derived cells re-migrating from foregut backtransplanted to vagal or sacral regions of host embryos. Dev. Dyn. 196, 217 – 233. Rubin, E., 1985. Development of the rat superior cervical ganglion: ganglion cell maturation. J. Neurosci. 5, 673 – 684. Sang, Q., Young, H.M., 1996. Chemical coding of neurons in the myenteric plexus and external muscle of the small and large intestine of the mouse. Cell Tissue Res. 284, 39 – 53. Santiago, A., Erickson, C.A., 2002. Ephrin-B ligands play a dual role in the control of neural crest cell migration. Development 129, 3621 – 3632. Schafer, K.H., Mestres, P., 1999. The GDNF-induced neurite outgrowth and neuronal survival in dissociated myenteric plexus cultures of the rat small intestine decreases postnatally. Exp. Brain Res. 125, 447 – 452. Schilling, T.F., Kimmel, C.B., 1994. Segment and cell type lineage restrictions during pharyngeal arch development in the zebrafish embryo. Development 120, 483 – 494. 13 Schneider, C., Wicht, H., Enderich, J., Wegner, M., Rohrer, H., 1999. Bone morphogenetic proteins are required in vivo for the generation of sympathetic neurons. Neuron 24, 861 – 870. Seaman, C., Anderson, R., Emery, B., Cooper, H.M., 2001. Localization of the netrin guidance receptor, DCC, in the developing peripheral and enteric nervous systems. Mech. Dev. 103, 173 – 175. Serbedzija, G.N., Bronner-Fraser, M., Fraser, S.E., 1989. A vital dye analysis of the timing and pathways of avian trunk neural crest cell migration. Development 106, 809 – 816. Serbedzija, G.N., Burgan, S., Fraser, S.E., Bronner-Fraser, M., 1991. Vital dye labelling demonstrates a sacral neural crest contribution to the enteric nervous system of chick and mouse embryos. Development 111, 857 – 866. Shepherd, I.T., Raper, J.A., 1999. Collapsin-1/semaphorin D is a repellent for chick ganglion of Remak axons. Dev. Biol. 212, 42 – 53. Shepherd, I., Luo, Y., Raper, J.A., Chang, S., 1996. The distribution of collapsin-1 mRNA in the developing chick nervous system. Dev. Biol. 173, 185 – 199. Song, H., Poo, M., 2001. The cell biology of neuronal navigation. Nat. Cell Biol. 3, E81 – E88. Taraviras, S., Marcos-Gutierrez, C.V., Durbec, P., Jani, H., Grigoriou, M., Sukumaran, M., Wang, L.C., Hynes, M., Raisman, G., Pachnis, V., 1999. Signalling by the RET receptor tyrosine kinase and its role in the development of the mammalian enteric nervous system. Development 126, 2785 – 2797. Tennyson, V.M., Payette, R.F., Rothman, T.P., Gershon, M.D., 1990. Distribution of hyaluronic acid and chondroitin sulfate proteoglycans in the presumptive aganglionic terminal bowel of ls/ls fetal mice: an ultrastructural analysis. J. Comp. Neurol. 291, 345 – 362. Tollet, J., Everett, A.W., Sparrow, M.P., 2001. Spatial and temporal distribution of nerves, ganglia, and smooth muscle during the early pseudoglandular stage of fetal mouse lung development. Dev. Dyn. 221, 48 – 60. Tollet, J., Everett, A.W., Sparrow, M.P., 2002. Development of neural tissue and airway smooth muscle in fetal mouse lung explants: a role for glialderived neurotrophic factor in lung innervation. Am. J. Respir. Cell Mol. Biol. 26, 420 – 429. Towers, P.R., Woolf, A.S., Hardman, P., 1998. Glial cell line-derived neurotrophic factor stimulates ureteric bud outgrowth and enhances survival of ureteric bud cells in vitro. Exp. Nephrol. 6, 337 – 351. Trupp, M., Ryden, M., Jornvall, H., Funakoshi, H., Timmusk, T., Arenas, E., Ibanez, C.F., 1995. Peripheral expression and biological activities of GDNF, a new neurotrophic factor for avian and mammalian peripheral neurons. J. Cell Biol. 130, 137 – 148. Trupp, M., Arenas, E., Fainzilber, M., Nilsson, A.S., Sieber, B.A., Grigoriou, M., Kilkenny, C., Salazar-Grueso, E., Pachnis, V., Arumae, U., 1996. Functional receptor for GDNF encoded by the c-ret proto-oncogene. Nature 381, 785 – 789. Trupp, M., Belluardo, N., Funakoshi, H., Ibanez, C.F., 1997. Complementary and overlapping expression of glial cell line-derived neurotrophic factor (GDNF), c-ret proto-oncogene, and GDNF receptor-alpha indicates multiple mechanisms of trophic actions in the adult rat CNS. J. Neurosci. 17, 3554 – 3567. Wang, H.U., Anderson, D.J., 1997. Eph family transmembrane ligands can mediate repulsive guidance of trunk neural crest migration and motor axon outgrowth. Neuron 18, 383 – 396. Wang, H.U., Chen, Z.-F., Anderson, D.J., 1998. Molecular distinction and angiogenic interaction between embryonic arteries and veins revealed by ephrin-B2 and its receptor Eph-B4. Cell 93, 741 – 753. Wehrle-Haller, B., Weston, J.A., 1997. Receptor tyrosine kinase-dependent neural crest migration in response to differentially localized growth factors. BioEssays 19, 337 – 345. Wingerd, K.L., Goodman, N.L., Tresser, J.W., Smail, M.M., Leu, S.T., Rohan, S.J., Pring, J.L., Jackson, D.Y., Clegg, D.O., 2002. Alpha 4 integrins and vascular cell adhesion molecule-1 play a role in sympathetic innervation of the heart. J. Neurosci. 22, 10772 – 10780. Wong, K., Park, H.T., Wu, J.Y., Rao, Y., 2002. Slit proteins: molecular 14 H.M. Young et al. / Autonomic Neuroscience: Basic and Clinical 112 (2004) 1–14 guidance cues for cells ranging from neurons to leukocytes. Curr. Opin. Genet. Dev. 12, 583 – 591. Yan, H., Newgreen, D.F., Young, H.M., 2003. Developmental changes in neurite outgrowth responses of dorsal root and sympathetic ganglia to GDNF, neurturin and artemin. Dev. Dyn. 227, 395 – 401. Yan, H., Bergner, A.J., Enomoto, H., Milbrandt, J., Newgreen, D.F., Young, H.M., 2004. Neural Cells in the esophagus respond to glial cell line-derived neurotrophic factor and neurturin, and are Ret-dependent. Dev. Biol. (in press). Yntema, C.L., Hammond, W.S., 1954. The origin of intrinsic ganglia of trunk viscera from vagal neural crest in the chick embryo. J. Comp. Neurol. 101, 515 – 541. Young, H.M., Newgreen, D., 2001. Enteric neural crest-derived cells: origin, identification, migration, and differentiation. Anat. Rec. 262, 1 – 15. Young, H.M., Hearn, C.J., Ciampoli, D., Southwell, B.R., Brunet, J.F., Newgreen, D.F., 1998. A single rostrocaudal colonization of the rodent intestine by enteric neuron precursors is revealed by the expression of Phox2b, Ret, and p75 and by explants grown under the kidney capsule or in organ culture. Dev. Biol. 202, 67 – 84. Young, H.M., Ciampoli, D., Hsuan, J., Canty, A.J., 1999. Expression of ret-, p75(NTR)-, Phox2a-, Phox2b-, and tyrosine hydroxylase-immunoreactivity by undifferentiated neural crest-derived cells and different classes of enteric neurons in the embryonic mouse gut. Dev. Dyn. 216, 137 – 152. Young, H.M., Hearn, C.J., Farlie, P.G., Canty, A.J., Thomas, P.Q., Newgreen, D.F., 2001. GDNF is a chemoattractant for enteric neural cells. Dev. Biol. 229, 503 – 516. Young, H.M., Jones, B.R., McKeown, S.J., 2002. The projections of early enteric neurons are influenced by the direction of neural crest cell migration. J. Neurosci. 22, 6005 – 6018.