* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Why do muscles shorten? 112ch11
Cell culture wikipedia , lookup
List of types of proteins wikipedia , lookup
Cell encapsulation wikipedia , lookup
Extracellular matrix wikipedia , lookup
Cellular differentiation wikipedia , lookup
Tissue engineering wikipedia , lookup
Organ-on-a-chip wikipedia , lookup
Cytokinesis wikipedia , lookup
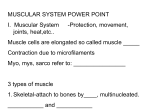
Why do muscles shorten? • What is the sliding filament theory of contraction? • How are myofibers organized? • What is the structure and function of actin, myosin and troponin? • Why do we “see” striations when we look through a light microscope? • What limits the degree of shortening in a sarcomere? • What is a muscle “twitch”? • How does a muscle create “All or None” and “Graded” responses? • What are the phases of muscle contraction? • Compare and Contrast smooth, skeletal and cardiac muscle The “Sliding Filament Theory” describes how two proteins called actin and myosin interact to shorten sarcomeres and the muscle to generate force. • THE BASICS: • Myosin tails and the Myosin Head• Thick filaments- • Thin Actin and troponin• Function of Calcium and troponin• The function of ATP• Ratchet Action and shortening: • What happens during rigormortis? Microscopic view of skeletal muscle How do these parts create a contraction? A single myosin filament has a tail that is fixed and a head that flexes. Many myosin filaments fit together to make the thick filaments Myosin heads bind actin fimaments, only if TROPONIN does not cover actin. Normally very little calcium is present and troponin is attached to actin (myosin blocked). Calcium binds troponin causing tropomyosin to move away from actin. Actin is now exposed and the myosin heads can bind to actin and a contraction begins if ATP is available (energy) to flex the myosin heads. Many actins bind with many myosin heads on the thick filaments during a contraction. One Sarcomere=Z-line to Z-line with actin/mysin/actin in between. Sarcomeres consist of all the actin and myosin found between two Z-lines. Sarcomeres shorten during a contraction. Striations look like this at really high magnification. “Myofibrils” are organized groups of actin/myosin filaments inside a myofiber. During contraction the opposing Z-lines are drawn closer together by the ratcheting action of the myosin heads along the actin filaments. TITAN-myosin to Z-line Ratcheting of myosin heads across actin shortens the myofiber! As the sarcomeres shorten, the z-lines (discs) get closer, eventually crunching into myosin. This crunch prevents further shortening and limits the maximum contraction (muscle shortening)! Cardiac Muscle functions in a manner similar to that of skeletal muscle with a few exceptions. Cardiac cells depolarize for long periods and do not have the quick twitches that are characteristic of skeletal muscle Cardiac cells are linked by Gap Junctions so when Na+ enters a cell it can cross into and depolarize the next cell and so-on. While each skeletal myofiber requires a depolarization from a synapse, cardiac cells can depolarize (heart beats) independently of the nervous system. (Take it out and watch it beat autorhythmically) • CARDIAC Muscle cannot undergo tetany ! Cardiac myocytes have a pacemaker potential and autorhythmicity! Their membranes become leaky to Na+ and K+ such that it causes “pacemaker” cells to depolarize. We call this pacemaker activity autorhythmicity. The depolarization is passed on to all neighbors via gap junctions and so on to all the cells of the heart. The autonomic nervous system serves simply to modify the function of the pacemaker cells (heart rate) and the amount of Ca++ that enters during contraction (force of contraction). Cardiac cells work 24/7 so they need more ATP and have more mitochondria than the typical skeletal muscle cell. Smooth Muscle cells contain actin and myosin, but are quite different from skeletal and cardiac myocytes. 1) Where do we find smooth muscle under involuntary control? 2) Smooth Muscle usually comes in flat sheets or tubes with cells that may or may not be connected by gap junctions. 3) The gut and artery have both circular and longitudinally arranged sheets of smooth muscle to complement each others function. Function of circular fibers Function of longitudinal fibers 4) In smooth muscle cells the actin and myosin are not organized into sarcomeres, but more loosely attached to the plasma membrane and sarcoplasm (no striations) 5) Smooth Muscle can generate force that is sustained for a longer time and uses less ATP (its cells typically have fewer mitochondria and rely more on glycolysis) 6) Smooth muscle is stimulated by the autonomic NS at a classic synapse (Multi-unit) or via a series of varicosities from a single axon (Single-Unit) where gap junctions carry depolarization to neighboring cells. Smooth muscle cells are found in blood vessels, glands, guts,and other places. SMCs contract using calcium entry/calmodulin binding as a signal to activate myosin light chain kinase (MLCK). MLCK phosphorylates myosin letting it bind actin and contract. Once the myosin in smooth muscle is phosphorylated it binds actin and the cell contracts, contraction ends when Ca++ leaves the cell and MLC-phosphatase removes the phosphate from MYOSIN…leading to SMC relaxation Smooth Muscle Applications: Asthma: excess constriction of airways Solution: promote dilation (reduce SMC contraction) High Blood Pressure: Excess contraction of blood vessel Solution: vasodilator drugs Low Blood Pressure: Not enough SMC tone in blood vessels. Solution: vasoconstrict blood vessels to push blood back to heart Peristaltic Waves in intestine: propel chyme, often the contractions are not strong enough (constipation)…what is the solution? Hypermotile Intestine (Diarrhea): Solution is to reduce intestinal SCM contractile force Hyperactive Bladder: improve receptive relaxation