* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download heart rate
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Myocardial infarction wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Artificial heart valve wikipedia , lookup
Electrocardiography wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
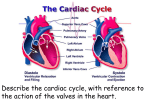
Vital Signs: Pulse & Heart Rate Video 1.1: Basic Heart Anatomy The Heart’s Location within the Thoracic Cavity - The heart is a hollow, muscular, cone-shaped organ o General location a. Positioned in the mediastinum (explain what this means!) b. within the _____________ cavity c. between the _________ cavities o enclosed by the pericardium a. function –____________________ - Esophagus and trachea are posterior to the heart The Heart’s Internal Structure - 4 chambers, or compartments o Two superior chambers, or _________ o Two inferior chambers, or ___________ o To prevent mixing of blood between chambers-- interatrial septum and interventricular septum Ventricular walls are thicker than atrial walls because they are responsible for pumping blood into the systemic and pulmonary circulations o Right atrium Receives deoxygenated blood from the body from three vessels Explain the functions of each of the following vessels in terms of where they carry blood to/from. 1. Superior vena cava 2. Inferior vena cava 3. Coronary sinus From the right atrium, blood goes to the right ventricle o Right ventricle Pumps deoxygenated blood into the pulmonary trunk o Left atrium receives oxygenated blood via the __________ veins o Left ventricle Pumps oxygenated blood into the aorta Left ventricular walls are __________ than right ventricular walls because they need to contract with more force in order to send blood throughout the systemic circulation - The systemic circulation supplies the tissues and organs of the body with oxygenated blood o the newly deoxygenated blood returns to the right atrium by the superior vena cava, inferior vena cava, and coronary sinus Video 1.2a: Your Beating Heart The Heart at a Microscopic Level - 2 functional units (syncytia): o the atrial syncytium o the ventricular syncytium o Atria contract, then ventricles contract, then the heart relaxes - Two types of cells in the heart wall o Contracting cells o Cells that generate an electrical signal (what is their role?) Form the cardiac conduction system: Occurs in each heartbeat The Cardiac Conduction System - Starts at the _________ node (SA node) o Location: _________ o Part of the cardiac conduction system that generates an electrical signal most rapidly o Spreads signal over entire atrial syncytium causing atrial contraction - Signal spreads to the ____________node (AV node) - Signal passes through the atrioventricular bundle (AV bundle) - Signal arrives in the interventricular septum o Passes through two bundle branches (right and left) - At apex, the fibers branch extensively, forming Purkinje fibers - Electrocardiograms (ECGs) assess the cardiac conduction system o Determine if electrical activity of the heart is working properly Video 1.2b: ECG Demo - ECGs are devices we use to detect the electrical activity in the heart o Electrodes are placed on the body 2 upper limb leads (Where do you attach them to the body?) 2 lower limb leads (where do you attach them?) 6 precordial leads (explain where they are attached to the patient). Allows you to look at the heart from 12 different angles-> can pinpoint location of abnormality, if present - The current arising from the SA node is a positive current, called depolarization o The positive current passes through the atrial walls o A negative current restores the electrical potential of the atrium back to normal after the passing of the positive current, this is called repolarization - Normal Sinus Rhythm (explain the shape/size of each wave). o P wave: first wave o QRS group of waves complex: second Consists of the Q, R, S waves o T Wave: third wave o Isoelectric lines –occur when there is no change occurring in the electrical state of the heart (i.e., no depolarization or repolarization is occurring) Between P wave and QRS complex Between QRS complex and T wave Video 1.3a: Heart Valves, Part 1 - Heart valves ensure that blood flows in one direction through the heart o Composed of dense, fibrous connective tissue o covered in endocardium- function?__________ - Heart has 4 valves- organized as two pairs o Atrioventricular valves (AV valves) Location: ____________ tricuspid valve mitral valve: Close when ventricles contract and the pressure in the ventricles exceeds pressure in the atria chordae tendinae: function:___________ papillary muscles contract along with ventricles, creating tension in the chordae tendinae, preventing the free edges of the valves from swinging upward into the atria Open after ventricular relaxation, when atrial pressure exceeds ventricular pressure o Semilunar valves (SL valves) Video 1.3b, Heart Valves, Part 2 - Blood passes from right ventricle to the pulmonary trunk and from the left ventricle into the aorta o Semilunar valves: pulmonic valve:______ aortic valve:__________ When closed, the cusps fall into the center of the pulmonary trunk and aorta to prevent backflow of blood from the vessel into the ventricle When the ventricles contract, pressure in them increaseswhen ventricular pressure exceeds pressure in the aorta and pulmonary trunk, the semilunar valves open When the ventricles relax, pressure drops- when the ventricular pressure falls below the pressure in the aorta and pulmonary trunk, the semilunar valves close Movement of valves during the cardiac cycle - When the heart is relaxed o the semilunar valves are closed and the AV valves are open blood is coming back to the right atrium through the superior vena cava, inferior vena cava and coronary sinus On the left side, blood is returning to the heart from the pulmonary veins from the lungs - Atria contract o Pressure in atria increases - Atria relax, ventricles contract o Pressure in ventricles exceeds pressure in atria o Pressure continues to climb as ventricles continue to contract -> ventricular pressure exceeds pressure in aorta and pulmonary trunk - Ventricles stop contracting, start to relax - Cycle repeats - When valves close, they cause vibrations to occur in the blood that’s passing through the heart o Vibrations are carried to the body’s surface and can be heard with a stethoscope o sound one:_________ o sound two:___________ Video 1.3c, Assessing Heart Rate Demo - Auscultation: - The heart is positioned deep to the sternum, slightly to the left of the midline in the chest cavity o the apex: Location: Orientation: point of maximal impulse- the most accurate place to check heart rate - Feeling the heart rate, or palpating, assesses the number of beats per minute - Auscultation allows assessment of heart rate as well as heart sounds o Heart sounds include sound one and sound two, usually called S1 an S2 S1 S2 - Physicians often auscultate in multiple locations to assess heart sounds related to the specific valves o aortic valve: _____ o pulmonic valve:____ o tricuspid valve: ____ o mitral valve: ______ - If a valve does not close all of the way, it will make a swishing sound - If a valve does not open all of the way, it will make a clicking sound Video 1.4a, The Cardiac Cycle, Part 1 Electrical Changes During the Cardiac Cycle - Conduction system: o Starts at the SA node Excitation of the atria creates the P-wave on an ECG o Signal sent to the AV node Delayed for 1/10th of a second— o Passed to AV bundle The only electrical connection between the atrial syncytium and ventricular syncytium o Excitation of the ventricles creates the QRS complex on an ECG o Heart relaxes, ventricles repolarize Creates the T wave on the ECG - These electrical signals create changes in the contracting cells, triggering muscle contraction Video 1.4b: The Cardiac Cycle, Part 2 Pressure Changes During the Cardiac Cycle - Pressure changes in the heart cause the valves to open and close, to prevent backflow of blood o The P wave on an ECG is followed closely by an increase in atrial pressure atrial contraction, atrial systole After atrial systole, the atria contract and pressure remains low o The QRS complex on an ECG is followed almost immediately by an increase in ventricular pressure The period of ventricular contraction is called ventricular systole When ventricular pressure exceeds aortic pressure, the semilunar valves open Once this pressure peaks, the ventricles stop contracting o Pressure in ventricles falls below the pressure in the aorta and pulmonary trunk The ventricles continue to relax and ventricular pressure continues to fall o When this pressure falls below atrial pressure, the AV valves open o The period when the ventricles are relaxed is called ventricular diastole –during this phase, ventricles fill with blood Ventricular Volume During the Cardiac Cycle - Ventricular volume is fairly high during relaxation, or diastole - During atrial systole- a little more blood is pushed into the ventricles, so the volume increases slightly - Ventricles contract, pressure increases and volume decreases o Blood is being ejected to the aorta and pulmonary trunk o AV valves open and ventricular volume begins to increase again Heart Sounds During the Cardiac Cycle o Heart sound one indicates the start of ventricular systole o Heart sound two indicates start of ventricular diastole Video 1.4c: Assessing Pulse Demo - Heart rate: - Pulse: o We assess pulse in elastic arteries, which can distend and retract o Pulse and heart rate are typically the same in a person with healthy cardiovascular function, but could be different if someone has poor peripheral circulation or arterial disease Locations to assess pulse: - carotid artery - brachial artery (at the antecubital fossa) - radial artery - femoral artery - dorsalis pedis - posterior tibial Video 1.5: Cardiac Output - Need to keep blood circulating through the body to supply the cells with oxygen and nutrients and to carry away metabolic waste products - Cardiac Output (CO) = the volume of blood ejected per minute o Influenced by heart rate (HR) and stroke volume (SV) o CO = HR x SV - Stroke volume: the volume of blood ejected during a single heartbeat o End diastolic volume (EDV): o End systolic volume (ESV): o Stroke volume = EDV - ESV - Cardiac output can be increased or decreased to meet the needs of the body - The autonomic nervous system plays a role in regulating cardiac output o Two branches: parasympathetic and sympathetic sympathetic division: in the heart, the sympathetic nervous system innervates SA node, AV node and the contractile cells of the myocardium when activated, causes the SA node to depolarize more quickly and can shorten the delay at the AV node o tachycardia = HR > 100 bpm sympathetic activation also causes contractile cells of myocardium to contract more forcefully -> leads to increased stroke volume parasympathetic division: in the heart, the parasympathetic nervous system innervates the SA node & the AV node parasympathetic nervous system slows the SA node’s rate of self-excitation o parasympathetic signals are carried to the SA node by the vagus nerve o bradycardia = HR < 60 bpm