* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Understanding MRSA (Methicillin resistant Staphylococcus aureus
Survey
Document related concepts
Transcript
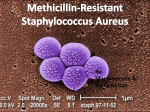
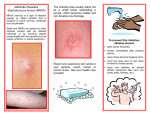
Understanding MRSA (Methicillin resistant Staphylococcus aureus) What is MRSA? Methicillin-resistant Staphylococcus aureus (MRSA) is a bacterium that causes infections in different parts of the body. It's tougher to treat than most strains of staphylococcus aureus -- or staph -- because it's resistant to some commonly used antibiotics. The symptoms of MRSA depend on where you're infected. Most often, it causes mild infections on the skin, causing pimples or boils. But it can also cause more serious skin infections or infect surgical wounds, the bloodstream, the lungs, or the urinary tract. Though most MRSA infections aren't serious, some can be life-threatening. Many public health experts are alarmed by the spread of tough strains of MRSA. Because it's hard to treat, MRSA is sometimes called a "super bug." A Closer Look at MRSA What causes MRSA? Garden-variety staph are common bacteria that can live on our bodies. Plenty of healthy people carry staph without being infected by it. In fact, 25-30% of us have staph bacteria in our noses. But staph can be a problem if it manages to get into the body, often through a cut. Once there, it can cause an infection. Staph is one of the most common causes of skin infections in the U.S. Usually, these are minor and don't need special treatment. Less often, staph can cause serious problems like infected wounds or pneumonia. Staph can usually be treated with antibiotics. But over the decades, some strains of staph -- like MRSA -- have become resistant to antibiotics that once destroyed it. MRSA was first discovered in 1961. It's now resistant to methicillin, amoxicillin, penicillin, oxacillin, and many other antibiotics. While some antibiotics still work, MRSA is constantly adapting. Researchers developing new antibiotics are having a tough time keeping up. Who gets MRSA? MRSA is spread by contact. So you could get MRSA by touching another person who has it on the skin. Or you could get it by touching objects that have the bacteria on them. MRSA is carried, or "colonized," by about 1% of the population, although most of them aren't infected. MRSA infections are most common among people who have weak immune systems and are living in hospitals, nursing homes, and other heath care centers. Infections can appear around surgical wounds or invasive devices, like catheters or implanted feeding tubes. Rates of infection in hospitals, especially intensive care units, are rising throughout the world. In U.S. hospitals, MRSA causes more than 60% of staph infections. Community-Associated MRSA (CA-MRSA) But MRSA is also showing up in healthy people who have not been living in the hospital. This type of MRSA is called community-associated MRSA, or CA-MRSA. The CDC reports that in 2007, 14% of people with MRSA infections had CAMRSA. Studies have shown that rates of CA-MRSA infection are growing fast. One study of children in south Texas found that cases of CA-MRSA had a 14-fold increase between 1999 and 2001. CA-MRSA skin infections have been identified among certain populations that share close quarters or experience more skin-to-skin contact. Examples are team athletes, military recruits, and prisoners. However, more and more CA-MRSA infections are being seen in the general community as well, especially in certain geographic regions. It's also infecting much younger people. In a study of Minnesotans published in The Journal of the American Medical Association, the average age of people with MRSA in a hospital or healthcare facility was 68. But the average age of a person with CA-MRSA was only 23. Top Picks How to Disguise Your Puffy Eyes What's Really in Your Shampoo? Baby Your Baby's Skin: Best Tips from the Experts Photos: 10 Psoriasis Triggers WebMD Medical Reference View Article Sources Reviewed by Debbie Bridges, MD on December 05, 2009 © 2009 WebMD, LLC. All rights reserved. ©2005-2007 WebMD, Inc. All rights reserved. WebMD does not provide medical advice, diagnosis or treatment. Original Article:http://www.mayoclinic.com/health/mrsa/DS00735 Definition Symptoms Causes Risk factors When to seek medical advice Tests and diagnosis Treatments and drugs Prevention Mayo Clinic Health Manager Get free personalized health guidance for you and your family. Get Started Free E-Newsletter Subscribe to receive the latest updates on health topics. About our newsletters Housecall Alzheimer's caregiving Living with cancer Enter e-mail Subscribe close window About our e-newsletters Free e-newsletters Mayo Clinic expertise We do not share your e-mail address Housecall, our weekly general-interest e-newsletter, keeps you up to date on a wide variety of health topics with timely, reliable, practical information, recipes, blogs, questions and answers with Mayo Clinic experts and more. Our biweekly topic-specific e-newsletters also include blogs, questions and answers with Mayo Clinic experts, and other useful information that will help you manage your health. Housecall Archives RSS Feeds close window Mayo Clinic Housecall Stay up to date on the latest health information. What you get Free weekly e-newsletter Mayo Clinic expertise Recipes, tools and other helpful information We do not share your e-mail address Sign up View past issues Definition MRSA infection is caused by Staphylococcus aureus bacteria — often called "staph." MRSA stands for methicillin-resistant Staphylococcus aureus. It's a strain of staph that's resistant to the broad-spectrum antibiotics commonly used to treat it. MRSA can be fatal. Most MRSA infections occur in hospitals or other health care settings, such as nursing homes and dialysis centers. It's known as health care-associated MRSA, or HA-MRSA. Older adults and people with weakened immune systems are at most risk of HA-MRSA. More recently, another type of MRSA has occurred among otherwise healthy people in the wider community. This form, communityassociated MRSA, or CA-MRSA, is responsible for serious skin and soft tissue infections and for a serious form of pneumonia. Symptoms Photos of staph infections Staph skin infections, including MRSA, generally start as small red bumps that resemble pimples, boils or spider bites. These can quickly turn into deep, painful abscesses that require surgical draining. Sometimes the bacteria remain confined to the skin. But they can also penetrate into the body, causing potentially lifethreatening infections in bones, joints, surgical wounds, the bloodstream, heart valves and lungs. Causes MRSA is a strain of staph that's resistant to the broad-spectrum antibiotics commonly used to treat it. Staph infections Staph bacteria are normally found on the skin or in the nose of about one-third of the population. If you have staph on your skin or in your nose but aren't sick, you are said to be "colonized" but not infected. Healthy people can be colonized and have no ill effects. However, they can pass the germ to others. Staph bacteria are generally harmless unless they enter the body through a cut or other wound, and even then they often cause only minor skin problems in healthy people. However, staph infections can cause serious illness. This most often happens in older adults and people who have weakened immune systems, usually in hospitals and long term care facilities. But in the past several years, serious infections have been occurring in otherwise healthy people in the community, for example athletes who share equipment or personal items. Antibiotic resistance Although the survival tactics of bacteria contribute to antibiotic resistance, humans bear most of the responsibility for the problem. Leading causes of antibiotic resistance include: Unnecessary antibiotic use. Like other superbugs, MRSA is the result of decades of excessive and unnecessary antibiotic use. For years, antibiotics have been prescribed for colds, flu and other viral infections that don't respond to these drugs, as well as for simple bacterial infections that normally clear on their own. Antibiotics in food and water. Prescription drugs aren't the only source of antibiotics. In the United States, antibiotics can be found in livestock. These antibiotics find their way into municipal water systems when the runoff from feedlots contaminates streams and groundwater. Germ mutation. Even when antibiotics are used appropriately, they contribute to the rise of drug-resistant bacteria because they don't destroy every germ they target. Bacteria live on an evolutionary fast track, so germs that survive treatment with one antibiotic soon learn to resist others. And because bacteria mutate much more quickly than new drugs can be produced, some germs end up resistant to just about everything. That's why only a handful of drugs are now effective against most forms of staph. Risk factors Because hospital and community strains of MRSA generally occur in different settings, the risk factors for the two strains differ. Risk factors for community-associated MRSA (CA-MRSA) Young age. CA-MRSA can be particularly dangerous in children. Often entering the body through a cut or scrape, MRSA can quickly cause a widespread infection. Children may be susceptible because their immune systems aren't fully developed or they don't yet have antibodies to common germs. Children and young adults are also much more likely to develop dangerous forms of pneumonia, which can result from CA-MRSA, than older people are. Participating in contact sports. CA-MRSA has affected sports teams. The bacteria spread easily through cuts and abrasions and skin-to-skin contact. Sharing towels or athletic equipment. CA-MRSA has spread among athletes sharing razors, towels, uniforms or equipment. Having a weakened immune system. People with weakened immune systems, such as those living with HIV/AIDS, are more likely to have severe CA-MRSA infections. Living in crowded or unsanitary conditions. Outbreaks of CA-MRSA have occurred in military training camps and in American and European prisons. Association with health care workers. People who are in close contact with health care workers are at increased risk of serious staph infections. In addition to these risk factors, CA-MRSA is also spreading through certain groups of gay men. A study published in the Annals of Internal Medicine found a new strain of MRSA spreading rapidly among gay men in Boston and San Francisco. For example, gay men in San Francisco were 13 times more likely to be infected than others in the city. Risk factors for health care-associated MRSA (HA-MRSA) A current or recent hospitalization. MRSA remains a concern in hospitals, where it can attack those most vulnerable — older adults and people with weakened immune systems, burns, surgical wounds or serious underlying health problems. This is particularly true if you have a hospital stay of more than 14 days. A 2007 report from the Association for Professionals in Infection Control and Epidemiology estimated that 46 out of every 1,000 people hospitalized are infected or colonized with MRSA. Living in a long term care facility. MRSA is also prevalent in these facilities. Carriers of MRSA have the ability to spread it, even if they're not sick themselves. Invasive devices. People who are on dialysis, are catheterized, or have feeding tubes or other invasive devices are at higher risk. Recent antibiotic use. Treatment with fluoroquinolones (ciprofloxacin, ofloxacin or levofloxacin) or cephalosporin antibiotics can increase the risk of HA-MRSA. When to seek medical advice Keep an eye on minor skin problems — pimples, insect bites, cuts and scrapes — especially in children. If wounds become infected, see your doctor. Signs and symptoms of a wound infection Redness, warmth and tenderness of the wound Pus — a yellowish-white fluid that may have a foul smell Fever Ask to have any skin infection tested for MRSA before starting antibiotic therapy. Some drugs that treat ordinary staph aren't effective against MRSA, and their use could lead to serious illness and more resistant bacteria. Tests and diagnosis Doctors diagnose MRSA by checking a tissue sample or nasal secretions for signs of drug-resistant bacteria. The sample is sent to a lab where it's placed in a dish of nutrients that encourage bacterial growth (culture). But because it takes about 48 hours for the bacteria to grow, newer tests that can detect staph DNA in a matter of hours are now becoming more widely available. In the hospital, you may be tested for MRSA if you show signs of infection or if you are transferred into a hospital from another health care setting where MRSA is known to be present. You may also be tested if you have had a previous history of MRSA. Treatments and drugs Both hospital- and community-associated strains of MRSA still respond to certain medications. In hospitals and care facilities, doctors often rely on the antibiotic vancomycin to treat resistant germs. CA-MRSA may be treated with vancomycin or other antibiotics that have proved effective against particular strains. Although vancomycin saves lives, it may become less effective as well. Some hospitals are already seeing strains of MRSA that are less easily killed by vancomycin. In some cases, antibiotics may not be necessary. For example, doctors may drain a superficial abscess caused by MRSA rather than treat the infection with drugs. Prevention Hospitals are fighting back against MRSA infection by using surveillance systems that track bacterial outbreaks and by investigating products such as antibioticcoated catheters and gloves that release disinfectants. Still, the best way to prevent the spread of germs is for health care workers to wash their hands frequently, to properly disinfect hospital surfaces and to take other precautions, such as wearing gowns and gloves when working with people infected with resistant bacteria. In the hospital, people who are infected or colonized with MRSA are placed in isolation to prevent the spread of MRSA. Visitors and health care workers caring for people in isolation may be required to wear protective garments and must follow strict hand-washing procedures. What you can do in the hospital Here's what you can do to protect yourself, family members or friends from health care-associated infections. Ask all hospital staff to wash their hands or use an alcohol-based hand sanitizer before touching you — every time. Wash your own hands frequently. Make sure that intravenous tubes and catheters are inserted under sterile conditions, for example, the person inserting them wears a gown, gloves and mask and sterilizes your skin first. What you can do in your community Protecting yourself from MRSA in your community — which might be just about anywhere — may seem daunting, but these common-sense precautions can help reduce your risk: Wash your hands. Careful hand washing remains your best defense against germs. Scrub hands briskly for at least 15 seconds, then dry them with a disposable towel and use another towel to turn off the faucet. Carry a small bottle of hand sanitizer containing at least 60 percent alcohol for times when you don't have access to soap and water. Keep personal items personal. Avoid sharing personal items such as towels, sheets, razors, clothing and athletic equipment. MRSA spreads on contaminated objects as well as through direct contact. Keep wounds covered. Keep cuts and abrasions clean and covered with sterile, dry bandages until they heal. The pus from infected sores may contain MRSA, and keeping wounds covered will help keep the bacteria from spreading. Shower after athletic games or practices. Shower immediately after each game or practice. Use soap and water. Don't share towels. Sit out athletic games or practices if you have a concerning infection. If you have a wound that's draining or appears infected — for example, is red, swollen, warm to the touch or tender — consider sitting out athletic games or practices until the wound has healed. Sanitize linens. If you have a cut or sore, wash towels and bed linens in a washing machine set to the "hot" water setting (with added bleach, if possible) and dry them in a hot dryer. Wash gym and athletic clothes after each wearing. Get tested. If you have a skin infection that requires treatment, ask your doctor if you should be tested for MRSA. Doctors may prescribe drugs that aren't effective against antibiotic-resistant staph, which delays treatment and creates more resistant germs. Testing specifically for MRSA may get you the specific antibiotic you need to effectively treat your infection. Use antibiotics appropriately. When you're prescribed an antibiotic, take all of the doses, even if the infection is getting better. Don't stop until your doctor tells you to stop. Don't share antibiotics with others or save unfinished antibiotics for another time. Inappropriate use of antibiotics, including not taking all of your prescription and overuse, contributes to resistance. If your infection isn't improving after a few days of taking an antibiotic, contact your doctor.