* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 01 lecture
Survey
Document related concepts
Transcript
Theme 01
Organization of nurse work of medical post and manipulation room
in Pediatric Hospital.
Deontological Aspects of Relationships of Health Care Providers With
Patients and Their Caregivers.
Medical deontology is a science about appropriate, about what should be the medical
employee and its relations with the patients and their kinsmen. The ethics study the moral norms
of the behaviour of person or of the social group. Specifically they distinguish a medical ethics.
The concept «medical deontology» is narrower, than concept «medical ethics».
The sources of formation of medical deontology and also of medical ethics (in particular,
doctor’s deontology and doctor’s ethics) are available in the works of the outstanding doctors of
the past – Hippocrat, Halen, Paracels, and in modern medicine – in works of М.Я. Мудров, С.
П. Боткин, В.А. Манассеин, Н.И. Пирогов etc.
The term «deontology» was entered in scientific turnover in the beginning ХIХ century
by the English Philosopher-Benthamite Jeremiah Bentham – for a designation of science about
professional behaviour of person. The basic principle of deontology is a conscious submission of
personal interests to interests of a society that is to super-personal interests.
It is possible to subdivide the norms of behaviour of medic on the: norms generalcultural (i.e. rules of human dialogue, what are base on the respect to human advantage), norm of
the etiquette (i.e. politeness, tactfulness etc., what are base on the habits of cultural behaviour
and traditions of dialogue between people), and norm medico-deontological (observance of these
norms provides trust of the patient to doctor, in their basis the requirements of medical trade lay).
It is possible among medico-deontological norm, in turn, to allocate the general-medical
and special norms. The general-medical norms are observed by all medical employments. The
specialmedical norms are realized in specific conditions of medical specialization, here,
accordingly, they are allocated deontology therapeutic, pediatric, surgical, stomatological etc.
The importance of the deontological side in the relations between doctor and the patient
grows constantly. It is caused by growing technical, tool equipment of modern medicine, by
tendency to differentiation and specialization of medical sciences and, thereof, by excessive
concentration of doctor’s attention on the separate struck with illness organs, and systems of the
organism
STUDENT (PHYSICIAN) – PATIENT MODELS OF COMMUNICATION
No matter how high the achievements and
technical possibilities of the modern medicine are,
a person will always wait and believe a doctor,
who can listen, approve and sympathize
Antoine de Saint Exupéry
One can’t treat the body without treating the soul
Socrates
Hippocrates wrote:
«There are three components in medicine: a patient, a
disease and a doctor... It is not easy for a patient to understand why his health gets better or
worse; it is the doctor who has to explain him everything». Francic
Maenab, the doctor of theology wrote:
«The doctor’s behaviour, his speaking manners play a significant role at the first encounter with
a patient».
Doctor’s professionalism does
not depend only on his knowledge of the etiology and pathogenesis of diseases, the methods of t
heir diagnosis and treatment but also on his ability to consult i.e.: to communicate, teach,
advise. The ability of the doctor to communicate determines his relationships with patients. Only
by gaining the patient’s trust and confidence, the doctor can get a detailed anamnesis; explain the
treatment requirements to patients. An experienced specialist expresses his opinions clearly
without causing anxiety. He is able to win patients’ favour and give hope to patients for positive
treatment. In the history of medicine trust and confidentiality are the basis for the doctor patient
communication.
In the last centuries the role of the doctor lay mostly in mere observation of the natural
course of diseases. Recently patients just entrusted doctors the right to make decisions. Doctors
“exceptionally for the patients’ sake” acted as they considered being necessary. It seemed that
such approach increased the treatment efficiency: the patient didn’t have any doubts or
uncertainties because the doctor took all the responsibility for his care. The doctor did not use to
share the information with the patient and hid the unpleasant truth.
Thus, in the realities of the modern world there is a high demand of new models of
doctor patient communication.
There are the following communication models between a physician and a patient:
Informative (a loyal physician, absolutely independent patient);
Interpretative (a persuasive physician);
Confidential (faith and mutual consent);
Paternal (a physician as a guardian).
The interpretative model is more suitable for the people with lack of education; the
confidential model is likely to be more appropriate for educated people who penetrate into health
problems essence.
The paternal model practiced earlier, can disturb a patient’s rights and is not used
nowadays with the exception of cases threatening a patient’s life or in case of operative or
rehabilitative emergency.
Nowadays a physician and a patient should collaborate; they are supposed to tell the
truth to each other and to share the responsibility for treatment efficacy. Such cooperation is
usually based on encouragement, understanding, sympathy and respect.
One of the most important conditions to maintain mutual understanding between a
physician and a patient is considered to be a sense of support. If a patient realizes that a
physician tends to assist, he will be more active during treatment and management.
If a physician displays understanding and a keen interest in a certain case, a person is
sure that his or her complaints are taken into consideration. This sense can be strengthened when
a physician says “I am listening to you and understand you”, confirming it by the expression of
his eyes or nodding assent.
Respect means to acknowledge that every person is of a great value. It should be taken
into consideration during the course of taking the history while a physician is learning the life
conditions of a patient.
Sympathy for a patient is a clue to close cooperation with him or her. It is worthwhile
for a physician to imagine himself as a certain patient. It is also very important to comprehend
and estimate the inner picture of the disease, that is to take into consideration not only a patient’s
subjective sensations but it is necessary to pay some attention to his state of health and selfobservation including his notion about the disease and its causes.
There are no strict rules of communication between a physician and a patient, though
all the health care workers in the world follow the general principles of deontology, medical
ethics of health professionals. A patient’s emotional state comfort is considered to be the true
criterion of deontology, that is the test to evaluate its effectiveness.
The oath, which is called Hippocratic, has its roots deep in the past. Later it was
transformed into a document containing a few special demands to be followed by physicians,
namely:
Keeping a medical secret;
Veto on the actions causing both moral and physical injury to a patient or his relatives;
Devotion to the profession.
The principle “Do not harm” is believed to be one of the most important in a
physician’s activity. This ancient Latin statement of medical ethics runs as follows: “primum
non nocere”. Each doctor is supposed to agree with the words by
Ye.Lambert: “There are
patients who cannot be helped, but there are no patients who would never be done harm”. It is
known that sometimes treatment seems to be more dangerous than a disease. That concerns the
side effects in simultaneous application of a great amount of them including incompatibility
between expected benefits and a possible risk due to medical measures.
A PHYSICIAN SHOULD BE ABLE NOT ONLY TO LISTEN TO HIS PATIENT, BUT
HE SHOULD BE ABLE TO HEAR HIM.
There is nothing more important than having a skill to hear his interlocutor. The
notion “to hear” means to perceive and comprehend the information. Egan wrote: “It is necessary
to hear not only by means of the ears, but also by means of the eyes, skin, mind, heart, that is to
put the soul into the process. A person does not simply perceive a sound; the words are coloured
with certain senses, they are able to stimulate imagination”.
The most important things can be transmitted via intonation, facial expression,
gestures, finally through silence.
The ability to hear includes:
Perceiving the information;
Perceiving senses;
Expressing sympathy;
Analysis.
Listen to your patient attentively not interrupting him. If necessary suggest some
leading questions, e.g. “You seem to be sad…..”, “You seem to be sad because of……”, “Has
anything serious happened?”, etc.
COMMUNICATION
Communication is supposed to be the information exchange among people. There are
5 main aspects of communication:
The person who transmits the message;
The information;
Mode of information transmission;
The person receiving the message;
Answer.
The main aspects that make communication easier:
Feeling sympathy for each other;
Mutual understanding;
Due time for communication;
Ability to speak clearly, not digressing from the subject.
RECOMMENDATIONS FOR PROVIDING THE MOST EFFECTIVE
COMMUNICATION WITH A PATIENT
At the beginning of the interview give a patient a kind smile.
Try to learn the causes of a patient’s subconscious anxiety. Help to solve the problem.
Try to give your patient a piece of advice, e.g. what he should do, expect, how he should
behave.
Never remind elderly people about their age, while speaking with them. The conversation
shouldn’t be in a hurry. The questions should be asked concretely, requiring only single-valued
answer.
Try to avoid giving only oral pieces of advice, write down recommendations as to
regimen, diet, medication therapy on a sheet of paper.
Try to explain the necessity of restriction of contracts with stimuli that damage psychics
(excessive informational loading, stresses, etc.).
At the first meeting:
smile friendly;
create natural atmosphere;
do not be in a hurry;
focus on a patient;
do not make an interrogation of the conversation, let the patient speak freely.
A good doctor possesses:
ability to empathize with;
thoughtfulness;
respectful attitude to the patient;
disquitness about the patient condition;
ability to keep patient confidentiality;
competence;
responsibility;
consideration.
A good doctor should:
demonstrate attitude towards the patient with a smile;
speak in a comprehensible language;
not abuse of medical terminology;
give distinct instructions;
avoid ambiguity;
not promise incredible things;
check whether the patient understood the information correctly;
be confident that the patient doesn’t have unaccountable questions any more.
Doctor-patient appointments usually have the character of a traditional consultation with
several defined stages. A doctor or a patient becomes the main character by turns.
Consultation stages
I
Main character – patient
Acquaintance, complaints
I
Main character – doctor
Anamnesis taking, physical examination
I
I
II
Doctor and patient are equal
Planning and prognosis of conservative
and operational treatment results
Environment plays an important role in the process of communication. Such details as
open door of the consulting room or surgery, unfriendly doctor’s facial expression can make a
great influence on the patient’s frankness. Hospital surrounding usually does not help with
‘physician-patient’ communication: it can oppress, make the patient feel helpless, because it is
difficult to seclude oneself in medical establishments. An excessive doctor’s full time job also is
harmful. The following notice was hanging on the Welsh doctor consulting room door: “When it
seems to you that I examine a patient too long, think about yourself at this place very soon.”
One more unbreakable rule should be pointed out: a conversation with a patient should be
face to face, the presence of a third person is excluded. Data about the patient older than 15 years
can’t be notified to extraneous people and even relatives without his\her consent. Keeping
patient confidentiality, as you remember, is one of the Hippocratic Oath statements.
A good doctor is associated not only with professionalism, encyclopedic knowledge,
calculated decisions and perfect medical procedure technique but with an ability to communicate
with a patient. Observations show that experienced doctors pay more attention to anamnesis
gathering and physical examination than to instrumental and research findings, which are less
important for such physicians. It is proved, that a correct diagnosis is made for 45-50 % of
patients on the basis of past history data and for 80 – 85 % on the basis of questionnaire and
physical methods of examination. Only for 15 – 20 % patients a profound laboratory and
instrumental research is needed to make correct diagnosis.
Unfortunately, doctors possess communicative skills “from time to time”. They are
obtained with the years of acquired experience. There are no special courses at medical
educational establishments that teach such skills. It’s a pity to see how doctors neglect the
conversation with a patient and use only laboratory instrumental diagnostics or carry out only
traditional treatment schemes. The art of conversation with a patient, ability to conduct a
dialogue with him or her calls for not only a desire to communicate but also some extent talent.
A doctor should possess a delicate psychological sense but regular work of
consciousness.
Successfull treatment is possible only in trustworthy human relationships and scientific
relationships. To reach this aim a technically equipped doctor should not only treat the patient
but communicate with him.
Is it possible to teach how to communicate correctly? Communicative skills can be
taught, they can be learnt but they can be forgotten very quickly, if not applied into practice
(Aspergen Med Teach, 1999). Communicative skills in relation to particular categories of
patients should be worked out to being automatic. Then a doctor will use them in routine and
dramatic situations. The use of modern didactic methods of teaching will assist students to
master communicative skills with a patient effectively.
Carrying into practice patient-oriented treatment, that implies frequent patient-doctor
contacts with high degree confidence formation to the latter, rises the quality of given medical
aid to great extent. (Lew in at al. Systematic Cochrane review, 2001).
The application of communication strategies by the teachers and tutors, explanation and
control of their usage by the students during practical part of classes at clinical subjects prepares
our students for real situations in their future practical activity.
By the initiative of L.Ya. Kovalchuk, PhD, Correspondent-member of Academy of
Medical Sciences of Ukraine, professor, Rector of I.Ya. Horbachevsky Ternopil State Medical
University “Student(Physician)–Patient” models of communication have been created.
Directions
Surgery, Oncology, Traumatology
Inner Medicine
Obstetrics and Gynecology
Pediatrics
Neurology and Psychiatry
COMPULSORY ELEMENTS OF COMMUNICATIVE SKILLS, WHICH SHOULD
BE TAKEN IN TO THE PRACTICAL PART OF THE OCCUPATION IN STUDYING OF
CLINICAL DISCIPLINES
How to work with the patient:
friendly facial expression when you see the patient at the first time and during
communication
greeting and introducing (name, level of competence, explanation or deciding the reason
of consultation, with the informed consent of the patient)
the establishment of trustworthy relationships (friendly facial expression, to show
interest, respect and care, corresponding style of communication)
gathering the anamnesis, reasonable substantiation of carrying corresponding physical
methods of examination
the explanation of examination findings and making plan for further actions
conversation accomplishment (verbal and nonverbal components)
II.
STANDARD
ALGORISMS
APPLICATION
OF
USING
COMMUNICATIVE
SKILLS IN SUCH SITUATIONS WITH TAKING INTO THE
CONSIDERATION THE PECULIARITIES OF CLINICAL DIRECTION ELABORATIONS
(SURGERY, INERNAL MEDICINE, OBSTETRICS, GYNECOLOGY, PEDIATRICS,
NEUROLOGY AND PSYCHIATRY):
while taking the anamnesis
while making physical methods of examination and perform medical procedures
while informing the examination findings
while planing and diagnosing conservative treatment findings
while substantiating reasonable surgical intervention
while informing about the findings of surgical intervention and possible post-operative
complications
while informing about the treatment prognosis
Objective structural clinical examination ( OSCE ) is not only an instrument for
students’ clinical skills assessment, but also for establishment of their communicative abilities.
III. COMPULSORY ELEMENTS OF COMMUNICATIVE SKILLS, WHICH
SHOULD BE TAKEN INTO THE STRUCTURE (OSCE):
Standard model of anamnesis and complaints taking
Example:
Complaints and anamnesis taking in children.
Friendly facial expression, smile.
Gentle tone of speech.
Greeting and introducing.
Tactful and calm conversation with sick child and his/her parents.
Further action explanation, (hospitalization and/or examination, etc.).
Conversation accomplishment.
Standard model of physical methods of examination and doctors’ procedures
Example:
Physical methods of children’s examination
1. Cordial facial expression, smile.
2. Gentle tone of speech.
3. Greeting and introducing.
4. Explain to a child and to his/her parents, which examination or procedures will be
carried out and get their informed consent.
5. Come in to contact with the child and try to get his/her thrust.
6. Prepare for examination or procedures carrying out (clean warm hands, warm
phonendoscope, use a screen if necessary).
7. Perform examination or procedures.
8. Explain examination findings to child’s parents.
9. Conversation accomplishment.
Estimating criteria in objective structural clinical examination (OSCE)
A student gets 1 point in case of correct usage of communicative model and
demonstration of perfect clinical skills.
A student gets 0.5 point in case of demonstration of perfect clinical skills and some
elements of communicative model.
A student gets 0 point in case of making mistakes in both models or in case of serious
mistakes in clinical skills performing.
“PHYSICIAN-PATIENT” COMMUNICATION MODELS
SURGICAL CLINIC
Complaints and anamnesis taking in surgical patients
Friendly facial expression, smile.
Gentle tone of speech.
Greeting and introducing.
Tactful and calm conversation with patient’s relatives, if it is necessary.
Explaination of planned actions of the patients’ treatment (hospitalization, performing
certain examinations, etc.).
Conversation accomplishment.
Physical methods of examination of surgical patients
Friendly facial expression, smile.
Gentle tone of speech.
Greeting and introducing.
Explain to a patient what examination will be performed and get his/her informed
consent.
Prepare yourself to perform examination (clean and warm hands, warm phonedoscope,
etc.).
Explain the necessity of transportation to the examination place (medical examination
room, ultrasonic investigation, computered tomography, endoscopy, etc.).
Perform examination.
Explain to the patient results of his/her lab tests correctly and accessibly.
Conversation accomplishment.
Informing about the results of examination.
Friendly facial expression, smile.
Gentle tone of speech.
Greeting and introducing.
Explain to a patient the results of his/her lab tests correctly and accessibly.
Involve patient’s relatives into the conversation (compare present examination results wit
h previous ones, clarify whether your explanations are clear for them).
Conversation accomplishment.
Complaints and anamnesis taking in postoperative surgical patients
Friendly facial expression, smile.
Gentle tone of speech.
Greeting and introducing.
Explain to a patient the aim of your visit, talk calm and tactful to the patient.
Get the patient’s agreement on bandaging.
Explain to the patient manipulation actions which are performed or will be performed in
the future and strategy of further treatment.
Conversation accomplishment.
Complaints and anamnesis taking in the postoperative proctological patients
Friendly facial expression, smile.
Gentle tone of speech.
Greeting and introducing.
Explain to a patient the aim of your visit, talk calm and tactful to the patient.
Explain to the patient how to perform hygienic procedures, bathes correctly, etc.
Get the patient agreement on bandaging.
Explain to the patient manipulation actions which are performed or will be performed in
the future and strategy of further treatment.
Inform the
patient with
a
stoma about possibility of further rehabilitation and improvement of life quality.
Conversation accomplishment.
Complaints and anamnesis taking in the postoperative vascular patients
Friendly facial expression, smile.
Gentle tone of speech.
Greeting and introducing.
Explain to a patient the aim of your visit, talk calm and tactful to the patient.
Get the patient agreement on bandaging.
Explain to the patient manipulation actions which are performed or will be performed in
the future and strategy of further treatment.
Conversation accomplishment.
Complaints and anamnesis taking in the postoperative thoracic patients
Friendly facial expression, smile.
Gentle tone of speech.
Greeting and introducing.
Explain to a patient the aim of your visit, talk calm and tactful to the patient.
Prepare yourself to perform examination (clean and warm hands, warm phonedoscope,
etc.).
Get the patient’s agreement on bandaging.
Explain to the patient manipulation actions which are performed or will be performed in
the future and strategy of further treatment.
Conversation accomplishment.
ORTHOPAEDIC AND TRAUMATOLOGY DEPARTMENT
Complaints and anamnesis taking in the inpatients
Friendly facial expression, smile.
Gentle tone of speech.
Greeting and introducing.
Calm and tactful conversation with patient’s relatives, if it is necessary.
Explain to a patient planned actions of his/her treatment (hospitalization, performing
certain examinations, etc.).
Conversation accomplishment.
Physical methods of examination
Friendly facial expression, smile.
Gentle tone of speech.
Greeting and introducing.
Explain to a patient what examination will be performed and get his/her informed
consent.
Prepare yourself to perform examination (clean and warm hands, warm phonedoscope,
etc.).
Explain to the patient the necessity of transportation to the examination place (medical
examination room, x-ray room, ultrasonic investigation, computered tomography, procedure
room, etc.).
Perform examination.
Explain to the patient results of his/her lab tests correctly and accessibly.
Conversation accomplishment.
While informing the results of examination.
Friendly facial expression, smile.
Gentle tone of speech.
Greeting and introducing.
Explain to a patient results of his/her lab tests correctly and accessibly.
Involve patient’s relatives into the conversation (compare present examination results wit
h previous ones, clarify whether your explanations are clear for them).
Explain to the patient the pecularities of his/her regimen (bed regimen).
Conversation accomplishment.
Complaints and anamnesis taking in the postoperative inpatients
Friendly facial expression and smile.
Gentle tone of speech.
Greeting and introducing.
Explain to a patient the aim of your visit, talk calm and tactful to the patient.
Get patient agreement on bandaging.
Explain to the patient actions concerning procedures, which were performed or are
planned to be performed in the future, the further treatment tactics.
Explain to the patient rehabilitation period peculiarities.
Conversation accomplishment.
ONCOLOGICAL CLINIC
Complaints and anamnesis taking in the inpatients.
Friendly facial expression and smile.
Gentle tone of speech.
Greeting and introducing.
Correct and calm conversation with patient’s relatives, if it is needed.
Explain to the patient what examination will be performed and get his/her informed
consent.
Conversation accomplishment.
Physical methods of examination of oncological patients
Friendly facial expression and smile.
Gentle tone of speech.
Greeting and introducing.
Explain to a patient, what examination will be performed and get his/her informed
consent.
Prepare yourself to perform examination (clean, warm hands, warm
phonendoscope, sterile gloves, etc.).
Explain to the patient the necessity of transportation to the examination place (medical
examination room, ultrasonic examination, X-ray or endoscopic room, etc.).
Make the examination.
Explain to the patient results of his/her lab tests correctly and accessibly.
Conversation accomplishment.
While informing the examination results and discussing the special treatment plan.
Friendly facial expression and smile.
Gentle tone of speech.
Greeting and introducing.
Explain to a patient results of his/her lab tests correctly and accessibly.
If the patient does not mind, involve his/her relatives into the conversation (compare
present examination results with the previous ones, make sure whether your explanation is clear
to them).
According to the results of clinical, lab and instrumental methods of examination devise
methods of special treatment for the patient. Inform the patient about the optimal combination of
special treatment methods, which are to be used. All drawbacks and possible complications of
each of the methods are to be discussed with the patient. If the patient refuses, the alternative
treatment methods should be offered.
Conversation accomplishment.
Complaints
,anamnesis
taking
and physical methods
of
examination in
patients of surgical department.
Friendly facial expression and smile.
Gentle tone of speech.
Greeting and introducing.
Explain to a patient the aim of your visit, talk calm and tactful to the patient.
Explain to the patient, who needs surgical interference, its necessity, inform him/her
about the possibility of stoma applying and assure him/her in the successful result of the
surgical operation.
Inform the patients, who underwent mastectomy, laryngectomy, limbs amputation, etc.,
about the possibility of prosthetic appliance and social rehabilitation. Patient with a stoma should
be informed about the results of stoma care, using urine and faeces collectors to improve the
quality of life.
Explain to the patient actions concerning procedures, which were performed or are
planned to be performed in the future, the further treatment tactics.
Get patient’s agreement on bandaging.
Conversation accomplishment.
Complaints and anamnesis taking in patients of radiological department.
Friendly facial expression and smile.
Gentle tone of speech.
Greeting and introducing.
Explain to a patient the aim of your visit, talk calm and tactful to the
patient.
Explain to the patient actions concerning procedures, which were performed or are
planned to be performed in the future, the further treatment tactics.
Explain to the patient how to take care of the skin or visible mucous parts properly to
prevent local ray influence.
Explain to the patient rules of radioprotective nutrition.
Get patient’s informed consent to participate in ray therapy treatment.
Conversation accomplishment.
Complaints and anamnesis taking in postoperative patients of thoracic department
Friendly facial expression and smile.
Gentle tone of speech.
Greeting and introducing.
Explain to a patient the aim of your visit, talk calm and tactful to the
patient.
Prepare yourself to perform examination (clean, warm hands, warm
phonendoscope, sterile gloves, etc.).
Explain to the patient actions concerning procedures, which were performed or are
planned to be performed in the future, the further treatment tactics.
In order to prevent complications, explain to the patient the principles of pleural drainage
and ways of managing it.
Get patient’s informed consent to participate in ray therapy treatment.
Conversation accomplishment.
ANAESTHESIOLOGY AND RESUSCITATION DEPARTMENT
Main principles of conversation and examination in patients, who requires first aid.
Before giving the first aid to a patient in critical condition, be sure in self safety. Be sure
that outer factors, which remain dangerous and may be harmful for the patient’s health, are not
available.
Follow the principles of asepsis and antisepsis. Use individual protection means (medical
gloves, masks, etc.).
If a patient is conscious, ask him/her: “How are you feeling?”
If you think that a patient is unconscious, touch his/her shoulder slightly and ask: “Are
you all right?” If, in case, the reaction of the patient is adequate, you may consider, that
respiratory tract functions normally, and there are no respiratory system and brain functions
disorders. Short answer of the patient shows that his/her respiratory tract or CNS is damaged.
The absence of reactions in patient points at his critical state. In this case check up the
presence of respiration, pulse, state and reaction of the pupils on the light. If signs of clinical
death are present, start intensive care immediately.
If you certify state of coma, come up to a patient at the back of his head, while examining
him, in order to:
а) have a posibility to provide immediate intensive care,
b) prevent yourself from damage (e.g. as a result of patient’s involuntary limb movement
in a state of extreme excitement, etc.).
It is necessary for a rescuer to have a full access to all parts of the patient’s body. If there
is no necessity, try not to touch the certain parts of body (intimate), clothes (pockets), to
prevent anycomplaints from the patient or his/her relatives.
Do not leave a patient in a critical condition without medical supervision.
When
you undress a patient, be
careful
with
the valuable
things. Document their amount in presence of witnesses; later put them in a safe.
Complaints and anamnesis taking in the inpatients who needs intensive therapy
Friendly facial expression and smile.
Gentle tone of speech.
Greeting and introducing.
You should talk to patient’s relatives correctly and reasonably.
Explain to a patient your actions concerning him/her (the necessity of hospitalization,
certain examinations and manipulations, etc.), which are planned in future.
Complete the conversation wishing the patient to get better as quickly as possible.
Physical methods of examination of the inpatients who needs intensive therapy
Friendly facial expression and smile.
Gentle tone of speech.
Greeting and introducing.
Explain to a patient, what examinations will be carried out and get his/her informed
consent.
Prepare for the examination (clean warm hands, warm membrane of phonendoscope,
mask on the face, sterile gloves, etc.).
Explain to
the
patient
the
necessity
of
transporting to the
place of examination (examination room, US, computer tomography, endoscopic department,
etc.).
Make the examination of the patient as sparing as possible (in some cases – in
the restful state or state of medical anesthesia).
Explain to the patient your actions concerning him/her (the necessity of hospitalization,
certain examinations and manipulations, etc.), which are planned in future.
Complete the conversation wishing the patient to get better as quickly as possible.
Peculiarities of communication with the patient during the intraoperative period and in
case of his/her unconsciousness:
During the communication with the colleagues, take into consideration that
consciousness of a patient can be not fully eliminated. Therefore behave correctly, do not
allow sharp and/or categorical(negative for the patient) statements. Follow the classic principle
of ancient medicine: “De mortius aut bene, aut nihil”.
Complaints and anamnesis taking in the postoperative inpatients and in case of
oppressed consciousness
1. A student must form the ability to estimate patient’s state according to the certain
clinical manifestations and to find out critical disorders of vital functions (violations of the
external respiration , hemodynamics, CNS functions, etc.)
2. A student
must always be
ready
to take
some
urgent measures of
intensive therapy and resuscitation (providing of patency of airways, expiratory support,
venous access, etc.).
3. If there is some urgent situation a student have immediately to inform (with the help
of medical staff on duty, relatives of the patient or other patients) consultanting physician and, if
it is possible, to help him/her.
4. A student has
to
speak with a patient clearly and
loudly,
if it
is necessary, repeat the phrase once or twice, as consciousness of the patient can be oppressed.
CLINIC OF INTERNAL MEDICINE
Complaints and anamnesis taking in patients with internal diseases
Friendly facial expression and smile.
Gentle tone of speech.
Greeting and introducing.
4.
Take complaints and anamnesis in a patient.
5. Explain to the patient results of his/her lab tests correctly and accessibly.
6. Explain to the patient your actions concerning him/her (the necessity of hospitalization,
certain examinations and manipulations), which are planned in future.
7. Conversation accomplishment.
Physical methods of examination of patients with internal diseases
1. Friendly facial expression and smile.
Gentle tone of speech.
Greeting and introducing.
4. Explain
to a patient,
what examinations will
be carried
out and
get his/her informed consent.
5. Find a contact with the patient and make an attempt to gain his/her trust.
6. Inform about the possibility of appearing of unpleasant feelings during the
examination.
7. Prepare for the examination (clean warm hands, cut nails, warm phonendoscope, etc.).
8. Examination (demonstration of clinical skill).
9. Explain to the patient results of his/her lab tests correctly and accessibly.
10. Conversation accomplishment.
Informing about the results of examination of patients with internal diseases
1. Friendly facial expression and smile.
Gentle tone of speech.
Greeting and introducing.
4. Explain toa patient results of his/her lab tests correctly and clearly.
5. Involve
the patient into the conversation (compare present examination results
with previous ones, clarify whether your explanations are clearly understood).
6. Conversation accomplishment.
Planning and prognosing the results of the conservative treatment
1. Friendly facial expression and smile.
Gentle tone of speech.
3. Greeting and introducing.
4. Correct and clear explanation of necessery treatment directions.
5. Discuss with a patient the peculiarities of taking medicines, duration of their usage,
possible side effects; find out whether your explanations are clear for him/her or not.
6. Conversation accomplishment.
Informing about treatment prognosis
1. Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. Correct and clear explanation of the expected results of the planned treatment.
5. Discuss with the patient the importance of permanent treatment, observance of the
appointed treatment regimen, find out whether your explanations are clear for hin/her or not).
6. Conversation accomplishment.
CLINIC OF OBSTETRICS AND GYNAECOLOGY
Peculiarity of work in obstetrics and gynaecology in terms of communication
with the patients is a necessity of consideration of originality of faminine psychology, in
particular, psychology of expectant mother. By his actions, behavior and words a physician must
do everything, in order to provide an optimistic mood, confidence in rapid convalescence or
happy completion of pregnancy and delivery. It should be remembered that gynecological
problems deal with very delicate, quite often intimate sphere, that is why during conversation or
examination one should not injure a woman psychologically and physically. In examination
rooms must not be any strangers, the door must be closed, a physician must not be disturbed on
a conversation with a midwife or a nurse, to look through the papers which do not concern the
patient. Only on such conditions the atmosphere of trust is created between a physician and a
patient without which successful treatment is often impossible.
Taking anamnesis in pregnant, women in labor and postpartum women
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4.Specify, how to address to a patient, set a contact.
5.Correct questioning, especially in relation to the intimate details of
the anamnesis.
6.Complete the conversation, to thank for it, wish happy course and completion of
pregnancy.
Physical methods of examination of pregnant, women in labor and postpartum women
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4.Explain the necessity of examination, its purpose.
5.Explain the details of examination, their safety, possible feelings during it.
6. Wash hands, put on gloves. Before an external obstetric examination- warm the
hands.
7. Make an examination.
8. Inform about the completion of the examination.
Informing about the results of the examinations of the pregnant, women in labor and
postpartum women
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. Explain, what examination you will interpret, what it can testify about.
5. Inform about the result of the examination, explain it in an accessible form.
6. Calm a patient in the case of presence of pathological changes, inform
about
the further actions.
7. Assure in positive changes and favourable prognosis at implementation of all
of the medical recommendations.
Planning and prognosing the results of examinations of pregnant, women in labor and
postpartum women
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing. By words, facial expression create the atmosphere of trust.
4. Inform a patient about the necessity of each action.
5. Inform the patient about the expected result from each action.
6. Inform the patient that treatment will not injure the patient, will not influence
negatively on the functions of woman organism.
7. Assure the patient, that all of the prescriptions will be done in time, and she has to
fulfill the recommendations.
8. Get patient’s informed consent of to conduct a treatment.
Proving the expedience of operative treatment of pregnant, women in labor
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing. By words, facial expression create the atmosphere of trust.
4. With a calm facial expression, inform a patient that in this pathology operative
treatment is needed in order to have an active healthy child.
5. Explain the volume of operative interference in an accessible form.
6. Inform the patient about the results of the operative interference (negative and
positive).
7. Assure the patient, that by rehabilitation measures the disadvantages of operative
interference can be taken to the minimum.
8. Get patient’s informed consent.
Informing about the results of operative interference and possible postoperation
complications
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3. Greet, inquire about the feeling, mood.
4. Watch the intonation of the voice, it must correspond to what you want to say.
5. With a calm facial expression, inform about the performed operation, the possible
results (after caesarian section there is the scar on the uterus, it is not desirable to be pregnant for
the first three years).
6. Encourage a patient to convalescence, assure with a confidence in convalescence,
to mark changes for better.
7. Inform about the prophylactic measures of undesirable results of operative
interference.
8. Completing the conversation, once again underline the confidence in a good
prognosis.
Informing about the prognosis of treatment of pregnant, women in labor and
postpartum women
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3. Greet, inquire about the feeling, mood.
4. Watch the intonation of the voice, it must correspond to what you want to say.
5. In case of favorable prognosis, express pleasure, verbally and by a pleasant facial
expression, by the voice intonation assure the patient in it.
6. In the case of unfavorable prognosis verbally encourage the patient to fight
against illness, mark every positive symptom. Intonation and facial expression must not be very
optimistic, as it can cause mistrust.
7. At an aggressive conduct behave yourself calmly, support verbally every step of
the patient, directed on the fight against illness.
8. Assure, that a patient does not have any questions. Completing the conversation,
once again underline the positive changes.
Taking anamnesis in gynecological patients
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. Specify, how to address to a patient, set a contact.
5. Correct questioning, especially in relation to the intimate details of the anamnesis.
6. Complete the conversation, thank for it, wish happy course and completion of
pregnancy.
CLINIC OF INFECTIOUS DISEASES
Taking complaints and anamnesis
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. Show interest, respect and care.
5.Take complaints, anamnesis of illness and epidemiological anamnesis (contact with
infectious patients, home or wild animals, eating of poor quality meal, etc.) of a patient.
6. Explanation of actions (reasons for isolation and/or a hospitalization, necessity of
making certain methods of examinations and treatment) which are planned to be done in the
future.
7. Conversation accomplishment.
Physical methods of examination of patients with infectious diseases
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. Show interest, respect and care.
5. Get in touch with a patient and gain his/her confidence.
6. Explain to a patient what examination should be performed, its expedience, obtain
patient’s informed consent.
7. Warn of unpleasant sensations during the examination.
8. Get ready for examination (a mask if necessary, clean and warm hands, trimmed
nails, sterile gloves, warm necessary instruments, using the screen if needed, etc.).
9. Examination (displaying clinical skills).
10. Explaine to the patient results of his/her lab tests correctly and accessibly.
11. Conversation accomplishment.
CLINIC OF DERMATOLOGICAL AND VENEREAL DISEASES
Complaints and anamnesis taking
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. Show interest, respect and care.
5.Take complaints, anamnesis of illness and epidemiological anamnesis (contact with
infectious patients, home or wild animals, eating of poor quality meal, etc.) of a patient.
6. Explanation of the actions (reasons for isolation and/or a hospitalization, necessity
of making certain methods of examinations and treatment) which are planned to be done in the
future.
7. Conversation accomplishment.
Physical methods of examination
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. Show interest, respect and care.
5. Get in touch with a patient and gain his/her confidence.
6. Explain to the patient what examination should be performed and its expedience,
obtain patient’s informed consent.
7. Inform about unpleasant sensations during examination.
8. Get ready for examination (a mask if necessary, clean and warm hands, trimmed
nails, gloves, warm necessary instruments, using a screen if needed, etc.).
9. Examination (displaying clinical skills).
10. Explain to the patient results of his/her lab tests correctly and accessibly.
11. Conversation accomplishment.
PEDIATRIC CLINIC
Complaints and anamnesis taking in new-born and nursing babies
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. Tactful and calm conversation with the parents of sick child.
5. Explanation of future steps concerning a child (hospitalization, performing some
methods of examination, etc.).
6. Conversation accomplishment.
Physical methods of examination of new-born and nursing babies
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. Explain to the parents what examination should be performed and obtain their
informed consent.
5. Prepare for examination (clean and warm hands, warm phonendoscope, etc.).
6. Examination.
7. Explaining the results of examination to baby’s parents.
8. Conversation accomplishment.
Complaints and anamnesis taking in toddlers and preschoolers (children aged from 1 to
6 years)
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. By means of game playing find a contact with a child.
5. Tactful and calm conversation with the parents of sick child.
6. Explanation of future steps concerning the child (hospitalization, some methods of
examination, etc.).
7. Conversation accomplishment.
Physical methods of examination of toddlers and preschoolers
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. Explain to the parents what examination should be performed and obtain their
informed consent.
5. Find a contact with a child, try to gain his/her confidence.
6. Prepare for examination (clean and warm hands, warm phonendoscope,
etc.).
7. Examination.
8. Explaining the results of examination to child’s parents.
9. Conversation accomplishment.
Complaints and anamnesis taking in school-age children
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. Tactful and calm conversation with sick child and his/her parents.
5. Explanation of the further steps to a child and his/her parents (hospitalization,
some methods of examination, etc.).
6. Conversation accomplishment.
Physical methods of examination of school-age children
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. Explain to a child and his/her parents what examinations should be performed and
obtain their informed consent.
5. Find a contact with the child, try to gain his/her confidence.
6. Prepare youself for examination (clean and warm hands, warm phonendoscope, use
the screen if necessary, etc.).
7. Examination.
8. Explaining the results of examination to child’s parents.
9. Conversation accomplishment.
Informing about the results of examination
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. Explain to a child and his/her parents what examinations should be performed and
obtain their informed consent.
5. Involve adolescent
and
his/her relatives into the conversation (compare present examination results with previous
ones, clarify whether your explanations are clear for them or not).
6. Conversation accomplishment.
Planning and prediction of conservative treatment results
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. Explain to child’s parents the necessity of further treatment directions
correctly and accessibly.
5. Discuss with parents and their child the peculiarities of drugs intake, duration of
usage, side effects and find out whether they understand your explanations.
6. Conversation accomplishment.
Informing about the treatment prognosis
1.Friendly facial expression and smile.
2.Gentle tone of speech.
3.Greeting and introducing.
4. Correct and clear explanation of expected results of treatment.
5. Discuss with the parents and their child the importance of continuous treatment,
following the treatment scheme, make sure that your explanations are properly understood.
6. Conversation accomplishment.
CLINICS OF NEUROLOGY AND PSYCHIATRY
Communication with the patient and his/her relatives is essential part of the physician’
profession. Such communication builds up the patient’s confidence. Therefore, a special
attention should be paid to the physician’s clothes, hair style, shoes, hands, etc.
Complaints and anamnesis taking in patients
1. Friendly facial expression and smile.
2. Gentle tone of speech.
3. Greeting and introducing.
4. Find a contact with a patient, try to gain his/her confidence.
5. Correct inquest, listening to the patient’s explanations.
6. Conversation accomplishment.
Physical methods of examination
1. Friendly facial expression and smile.
2. Gentle tone of speech.
3. Greeting and introducing.
4. Find a contact with a patient, try to gain his/her confidence.
5. Explain to the patient the necessity of the examination and its aim, get his/her
informed consent.
6. Explain to the patient examination details, its safety and possible sensations.
7. Prepare for the examination (clean, warm hands, etc.).
Examination.
Explain to the patient results of his/her tests correctly and accessibly.
Conversation accomplishment.
Informing about the results of examination
1. Friendly facial expression and smile.
2. Gentle tone of speech.
3. Greeting and introducing.
4. Interpretation of test results.
5. Calm a patient in the case of presence of pathological changes, inform
about
the following actions.
6.
Assure in positive changes and favourable prognosis at implementation of all
of the medical recommendations.
7. Conversation accomplishment.
Planning and prognosing the results of the conservative treatment
1. Friendly facial expression and smile.
2. Gentle tone of speech.
3. Greeting and introducing.
4. Brief and clear explanation of the treatment necessity.
5. Discuss with a patient the peculiarities of drugs intake, duration of usage, side effects
and find out whether he/she understands your explanations.
6. Conversation accomplishment.
Informing about treatment prognosis
1. Friendly facial expression and smile.
2. Gentle tone of speech.
3. Greeting and introducing.
4. Correct and clear explanation of expected results of treatment.
5. In case of favorable prognosis, express pleasure, verbally and by a pleasant facial
expression, by the voice intonation to assure the patient in it.
6. In the case of unfavorable prognosis, try verbally to encourage the patient to fight
against illness, mark every positive symptom. Intonation and facial expression must not be very
optimistic, as it can cause mistrust.
7. At an aggressive conduct behaviour yourself calmly, support verbally every step
of the patient, directed on the fight against illness.
8. Discuss with the patient the importance of continuous treatment, following the
treatment scheme, make sure that your explanations are properly understood.
9. Assure, that the patient does not have any questions.
10. Complete the conversation, once again mark each positive symptom.
WORK IN THE CHILDREN'S HOSPITAL
Reception
The child directed to a hospital gets into a reception room where his initial examination
will be carried out.
The appointment card (= direction letter = referral note) may be given by the polyclinic
doctor, the specialist, or the family doctor; the patient may be delivered by the ambulance. Only
patients in severe condition can be accepted without an appointment card.
In an appointment card, the full name, age, permanent address, preliminary diagnosis, if
possible — the data of the carried out inspection, and also date, surname of the doctor and a
medical seal or a seal of the establishment are given. Besides, with the purpose of preventive
care of an infectious disease in the non-infectious hospital, the information about the child's
contact with infectious patients isnecessary to be indicated in the appointment card, as well as
possible infringements of stool ('yes' or 'no', if 'yes'"— then we should find when there was a
contact with an infected person, as each infectious disease has its own incubation period — this
is known by the doctor). At the presence of contact of a patient with a child with infectious
diseases (in case of obligatory hospitalization) He/She will be admitted in the special isolation
ward or will be transferred to the infectious department.
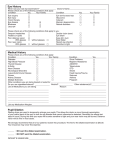
City children's hospital # 3 Appointment card
Borody Oleg lv., 2 years old, the address is: Solnitchnaya str., 14/92, goes on
hospitalization.
The diagnosis: Acute Bronchitis.
Iron deficient anemia of 1st degree.
The general blood analysis on 14.12.2010: RBC — 3.4 T/L, Hb — 92 g/L, WBC —
10 G/L, ESR — 12 mm/hour.
No contact with infectious patients, infringements of stool are not present.
15.12.2010
Sign, and stamp of local doctor
An appointment card to the children's hospital
If the child is delivered into the department without parents (in cases of accident, trauma,
sudden significant deterioration of the health state), the information of hospitalization should
urgently be told to the parents of the patient or the local police station should be informed for
the search of the parents in case the child's health is deteriorated.
In children's medical establishment, there is an independent reception with separate
medical personnels (doctors, nurses). In small children's hospitals, the child is accepted by the
doctors on duty in the children's branch or the pediatricians occupying the post of the doctor on
duty in the hospital, sometimes local doctors do it.
Reception of the patient should be carried out according to the following standard
obligatory plan
1.
Registration — First the nurse fills in the data concerning the patient in the
'Admission register' or 'hospitalization register', (date, full name, age of the child, the address,
the diagnosis in the appointment card) and draws up a passport part in the case history.
Simultaneously, the child's body temperature is measured and later examined by the
doctor on duty. The specified order is broken in case when a condition of the patient is severe
and demands urgent help.
2.
Doctor's examination (collection of complaints, the anamnesis of diseases and life,
the estimation of the child's condition, etc.) is carried out in approximately 20-30 minutes
depending on the disease and seriousness of the condition of the child. Then the doctor (in our
country personally) writes down all received data in the case history. At the end of this, the
preliminary diagnosis, a plan of the inspection of the patient and his treatment are indicated (the
list of medications and medical procedures).
3.
After examination by the doctor and the case history is filled, the nurse carryies
out the sanitary processing of the patient:
First of all, the hygienic condition of the child (by examination of the neck, ears and all
surface of the skin, nails on the fingers and toes, as well as the hair) is checked.
In case of long nails, they should be cut.
At diagnosis of pediculosis, the appropriate processing should be carried out.
Then, if necessary, according to the prescription of the doctor, the child takes a hygienic
bath or shower.
Attention! In case of severe condition of the patient, sanitary processing should be
carried out only after rendering the urgent help and with the permission of the doctor.
4.
After reception, the child is transferred to an appropriate department. The kind of
transportation is defined by the doctor depending on the condition of the patient:
• If the state of health of the child is satisfactory, then he/she can go to the
department independently under the nurse's supervision.
• Children of the first-second year of life are carried on hands.
• The medical staff transports heavy patients on stretcher, carriages (Fig. 3), etc.
• In absence of carriages, lift escalator or elevetor, the child of an advanced age
can be transferred on the bed sheets or blanket.
Transportation of the patient comes to an end with the case history and the prescription
form (the plan of treatment and inspection of the patient):
To a nurse from the child's department (if a condition of the patient is not severe, in
evening-night shift).
To the doctor on duty (in the afternoon; if the condition of the patient is very serious at
any time of the day).
If the child is under 1 year of age, feeding schedule is also prescribed. Besides, an
additional verbal communication with the department about the condition of the hospitalised
patient is necessary.
The
carriage
Simultaneously we shall consider kinds of possible transportation of the
patient outside the hospital (Attention! It may be only if the condition of the patient
allows transport him/her):
• By ambulance.
• Sanitary aircraft— by plane, helicopter (in mountainous place, for
urgent transportation to far distances).
• In emergency cases — any road transport.
Except the specified function of a reception room (reception of patients and
their hospitalization), it has one more function — the registration of the
movement of patients in a medical establishment. With this purpose, the medical
staff fills the following documents:
(a)
Hospitalization register.
(b)
In case parents refuse hospitalization, the data on the patient
are written down in special refusal register; besides, at refusal, in some
cases (such as infectious disease and severe condition of the child), the
doctor in the reception must inform the local doctor and the school where
the child studies (the kindergarten) about the situation.
(c)
Discharged register of the patients.
(d)
Register of transferring to other hospitals. For example: after
significant deterioration of the condition, the patient from the small city
hospital is transferred to reanimation department (= department of intensive
therapy = Intensive Care Unit — ICU) of the regional children's hospital,
the child from cardiological branch is transferred
to surgical branch in connection with the development of acute appendicitis,
etc. (e) Register of fatal cases.
It is clear that the list of patients in the 1st journal should be equal to the total amount of
patients in the last three registers.
Medical department
During all the time of stay in a hospital, the child is treated in the medical department. In
total, the hospital may have from 1 -2 up to 10 and more departments depending on its size. In
one children's department, there may be patients with different uncontageous diseases
(rheumatic fever, pyelonephritis, gastritis; in the same branch, only in a separate chamber,
patients with bronchitis, pneumonia, etc.). There are specialized hospitals in which children with
diseases of one system (cardiological, gastroenterological, hematological, etc.) are treated.
The main objective of all medical personnel in the department is an operative inspection
of the patient, the timely statement of the correct diagnosis and, at an opportunity, the full
treatment of the child or (in case of incurable disease) realization of the necessary complex of
medical actions for the patient.
Structure of the children's department
The department consists of isolated ward (= chamber = room — in some countries)
sections; for children of the 1st year of life, there should be no more than 24 beds, over one
year— not more than 30 beds. In one ward there may be accordingly 1-4 and 4-6 beds. The best
for the children of breast-feeding age are box wards, when every child has his own ward which
prevents possible infections to other patients. Till this time, in some hospitals, according to the
old rule there are wards which may not be very effective half-boxes with wooden- glass
partitions only between beds.
Hygienic requirements in wards are:
The distance between beds should not be less than 1.5 m.
Every child should have a personal bedside table and a case for clothes.
In each ward, one quartz lamp should be hung.
If there is no separate toilet near the ward, then the presence of a washbasin with
cold and hot water is necessary.
Generally, the structure of the children's department comprises of:
The department manager's room.
Duty room — a room for the doctors work.
A room of the senior nurse.
A post of the attendant nurse (on duty); for the convenience of constant
supervision, it is often located in corridors of the department; near the table of the
nurse, there are some hospital shelves in which the most necessary medicines and
medical tools are kept.
A post of the attendant (on
duty) nurse
In the department, there is nurse's room for inter-muscular injections, eye
dropping and other medical procedures, in which, by obligatory rules, medical products
and tools for manipulations are kept in the safe, refrigerator or in usual shelves.
A separate (!) manipulation room for intravenous injections.
In the branch, usually there is a special separate room for specific medical
procedures with the purpose of treatment and inspection (for example, for intubation of
the patient, examination by the ENT-doctor, the urologist, and the gynecologist, etc.).
A physical procedure cabinet (inhalation, electrophoresis, etc.).
A dining room.
A rest room for the doctor on duty.
Bathhroom.
A toilet (separate for medical staff and patients).
Sanitary-and-hygienic and anti epidemical regime
Sanitary-and-hygienic and anti epidemic regime is the extensive complex of actions
which are carried out by all employees of the medical personnel, and also by patients, the
purpose of it is maintaining cleanliness in the medical establishment and anticipation of future
epidemics of infectious diseases.
The following rules are included into the structure of these actions.
As it was mentioned above, in an appointment card, the doctor should specify the data
of the contact of the child with infectious patients.
Despite of the anamnesis written in the refferal form, a doctor at a hospital to which the
patient is reffered, has to enquire on the epidemiological anamnesis once more (see pg. 80). As
for the tactics of the doctor in case of the positive anamnesis you, students, already know it.
Even if the epidemiological anamnesis of the child is not aggravated, the patient needs to be
examined carefully in a reception to avoid an infectious pathology.
Sanitary procedures which should be primarily carried out at reception lasts during all the time
of stay of the patient in a hospital. If mother is in a hospital, then once a week, she will cary out
the procedures in place of a nurse. Every week each patient takes a hygienic bath.
In the department, bed sheets and clothes should be changed in due time. The frequency
of the change depends on the pathology, age of the child and his condition.
Furniture and the object of common use (couch and pillow on it) should be covered
with polyethylene film which is wiped up by 1% sol. of chloramines or 0.5% sol. of chloride of
lime 2 times after every patient, with an interval of 15 minutes, and after that with water. Sterile
disposable film sheets can be used. Simultaneously after every patient, the bed sheet on a couch
are changed.
The medical staff should observe the rules of preparation and distribution of food, and
patients — rules of eating food. Usually, it is prepared in a special room. After delivery to the
department, it is possible to keep food stuffs in a separate room not longer than 2 hours. Portions
are given into a dining room through a special window. The utensils are exposed to special
processing after use.
There should be drinking water for patients.
All workers of the department are obliged to observe the rules of personal hygiene, as
well as every patient is obliged to carry out all rules of personal hygiene.
One of the main anti-epidemic actions is disinfection which helps to
prevent the distributions of microbes of illnesses in the hospital and their destruction.
The disinfection can be:
a.
Preventive.
b.
Carried out in the epidemic center which is divided into:
Current.
Final.
Preventive disinfection is a complex of actions for preventing the accumulation and
distributions of activators of diseases in the hospital. Preventive disinfection should be carried
out by the following ways:
1. Ventilation of wards — four times a day.
2. Quartz (UVR) wards 2 times a day for 15 minutes.
3. Vacuum cleaning or shaking out in the fresh air of soft things (e.g. mattresses,
blankets, curtains, etc.).
4. The complex of preventive disinfection includes the above mentioned i ules of the
observance of hygiene by medical staff and patients, and also the rules of preparing and
distribution of food.
5. Wiping at least 2 times a day (in some departments — more often, for example, in
the infectious one — 4 times a day) the floor, windows, furniture. toys with specially
prepared solutions, for example:
(a) Chloride of lime (now rarely used) — fine powder of white color; it is necessary to
keep it in the dry pack protected from the light; only the patient's excrements are
disinfected with this dry powder. Chloride of lime in the liquid form is made and applied as
follows:
At the beginning, a special 10% or 20% solution is prepared (so-called 'clarified'): the
necessary quantity of the dry powder (for example, 1 kg to 10 L of 10% solution) is
stirred in a small amount of water; then gradually; water is added up to the necessary
volume (in this case — up to 10 L) and at constant stirring, till the formation of
homogeneous mix is achieved. The received structure is covered with a lid.
Approximately in 1 hour, the mix is mixed up once more, in 1 hour— once
again, and after 1 hour — once again; thus, within the first 3 hours it is mixed up 3
more times.
In 24 hours, from the beginning of manufacturing, the ready clarified solution
(in this case 10%) is poured out and then kept for no more than 7 days in enameled,
wooden, metal (protected from corrosion) well-closed basin.
Examples of calculation of the quantity:
~ 500 g of powder and water up to 5 L = 5 L of the 10% solution
~ 2 kg of powder and water up to 10 L = 10 L of the 20% solution
At work, the so-called working solution is used 0.5-1%, which is made
by the necessary dilution of the clarified solution. Examples of
calculation:
~ 1 L of the 10% main solution + 9 L of water = 10 L of the 1% working solution
~ 1 L of the 20% main solution + 19 L of water = 20 L of the 1% working solution
~ 500 ml of the 10% clarified solution + water (up to 10 L) = 10 L of the 0.5%
working solution
The working solution can be used no more than 24 hours.
For cleaning windows, the floor, furniture, toys, etc. 0.5% solution of chloride of lime is
used.
(b) Chioramines В (in dry form, it is a powder of white color) — for usage,
1% solution is made by gradual stirring of the necessary quantity of the powder, first in a
small volume of hot water (50-60°C), and then adding more and more water up to the necessary
full volume(for example: 50 g of powder and 5 L of water). To store a solution is possible no
more than 5 days.
(c) Dezaktin— dry powder mixed in water for 1-2 minutes, for the formation of 0.1-2.5%
solution which is used for the current and final disinfection. When water temperature is 60°C,
there will be an accelerated dissolution of the medium (for concentrations over 0.5%).
You can save 24 hours.
The current disinfection is a complex of actions for the reduction of infection in the whole
room near the centre of the infection. For example: in the child's department (non-infectious) on
the 1st floor of ward #4, a child who is hospitalized for the treatment of pneumonia, suffers from
salmonellosis as well; the current disinfection should be carried out on the territory of the whole
1st floor.
Three kinds of disinfection are applied:
1.
Chemical — for disinfecting toys, furniture, windows, the floor etc. with
disinfectant solutions of high concentration — 1% solution of chloride of lime and 2% solution of
Chioramines.
2.
Physical — boiling subjects (pans, dishes, etc.) in water; the addition of soda or
some laundry soap (10-20 g in 1 L of water) is effective.
3.
Mechanical— washing the linen, removal of dust and dirt with a damp duster.
The final disinfection is an utter elimination of the activator of a disease in the centre of
the infection (according to the given example, in ward # 4 it
is necessary to carry out not current, but final disinfection). Thus, the above mentioned
concentrated liquid disinfectant solutions, dry powder are used. Many subjects (footwear, books)
are processed in disinfection wards.
Louse infestations (= pediculosis) is an attribute of untidiness, infringement of the rules
of hygiene by a person, and also non-observance of the sanitary- and-hygienic regimen in a
hospital.
Let's recollect biology: three kinds of lice can parasitize a person — head, crab (= pubic)
and body (= clothes) louse (the name specifies the place of their localization); simultaneously
there may be nits (= eggs), larva and mature (- imago).
The survey on pediculation is done by the nurse in a reception room. As there are three
kinds of lice, the appropriate parts of the body and clothes of the patient are exposed to survey.
At detection of pediculosis, medical tactics can be different depending on the condition
of the patient:
1.
If the child is well (for example, parents brought him/her to the hospital
with the purpose of some non urgent operation), he/she is usually sent home for
elimination of lice, then hospitalization is allowed.
2.
If the child needs hospitalization, but his/her condition is not very serious,
in a separate room of a reception, the special processing of the patient should be carried
out, then the child is transported to the ward.
3.
If the condition of the patient is severe or very severe, first of all, the
treatment of the basic disease is carried out, and the processing is made after the
improvement of his/her condition and only with the permission of a physician (in this case, it is
necessary to observe special rules for the warning of distribution of lice among other patients,
especially before processing, — the patient is put into the separate ward, there should be a scarf
on his/her head, etc.).
The technique of eliminating process of the child at revealing head lice:
(a)
It is possible to shear hair (it is usually done with boys — an ideal momentary
way!) or to process the head of the patient with one of solutions used for such a purpose:
Lotions 'Nittifor', 'Miloca', 'Lanchet', special shampoos, etc.
(b)
After processing, the head is wrapped up with a polyethylene bag,
then a scarf is put on it; in such position, the child stays for 20-40 minutes (according to
the instruction).
(c)
Then, the head is washed by hot water with laundry soap.
(d)
The next moment is the most scrupulous one; it is gradual combing of the
patient's hair with a fine-tooth comb with a piece of cotton wool (moistened in 9% vinegar
solution).
(e)
The head is swilled with a lot of water.
Cut off hair, and the hairs cut should be put on an oilcloth and burnt. At revealing only
nits, it is possible to apply more simple solution: the hair is processed with warm (30°C) 9%
solution of vinegar, then for 15-20 minutes, the head is wrapped up with a scarf, after that, the
hair is combed out and the head is washed.
The clothes on which body lice are revealed should be packed into a polyethylene bag
and sent into the chamber for disinfection.
Special features of the medical personnel hygiene
Dear students, surely you know all the rules of personal hygiene of the medical
personnel, therefore they are only listed here: 9 Tidy appearance.
• A standard medical smock (coat).
• A cap or a kerchief on a head.
• Short nails.
• Special hospital footwear which is easily disinfected (for example, leather).
• Hands well washed up with soap.
• To medical sisters and doctors engaged in surgical manipulations, watches, rings,
varnish on nails are forbidden.
• According to indications (the maternity, infectious department, epidemic of
influenza, etc.) a mask is put on; it is necessary to change a gauze mask every 4 hours; at
an opportunity, it is better to use disposable sterile masks.
Rules of hygiene of patients in the children's hospital
The hygienic condition of the ill child is watched by mother and medical staff of
children's hospital.
The rules of personal hygiene of the patient older than 1 year include:
1. Care of the appropriate parts of the head and the trunk:
(a) Washing— 2 times a day, in the morning and in the evening, according to indications
(intake of food in horizontal position, the child in a serious condition, etc.) the amount of
washing procedures should be increased. This, as well as all other procedures, is carried out by a
matured child himself if he/she is not in a serious condition; the child in a severe condition is
washed by his/her mother or nurse.
(b) Cleaning teeth with a brush — 2 times a day; it is necessary to teach the child to
clean his/her teeth correctly: to move a tooth-brush on the vestibular and the lingual surfaces of
teeth from the top downwards and from below upwards from both sides; and on the surfaces of
the closure of the teeth.
(c) The sick child should rinse his/her mouth after each reception of food, especially
during diseases of the mouth (stomatitis, quinsy, pharyngitis); it is rational to rinse the mouth
with 1.5%-2.5% of soda or 1% of salt solution.
(d) It is necessary to wash ears every day.
If there is some ear-wax in the ear canals, the nurse cleans the patient's ears in the
following way: 3-5 drops of the 3% solution of hydrogen peroxide or sterile Vaseline oil are
instilled into the ear, after which the wax plug is removed with the help of cotton-buds.
(e) Eyes are washed without special assignment 2 times a day.
If the patient's eyes turn sour, eyelashes stick together, it is necessary to wash the eyes
with warm tea of strong concentration (brown color), moving a piece of gauze moistened with
tea, from(Attention!) an external corner up to the nose bridge.
(f) As for nostrils, the child of the advanced age usually clears them out
himself/herself.
With such a purpose, the nurse at first puts cotton-buds, moistened with oil solution
(Vaseline, Glycerin) into nasal cavity, then for 2-3 minutes, the head of the child is pushed
backwards, and then by rounding movements, clears nostrils. The nostrils are processed one by
one.
(g) The individual comb should be used for daily care of hair according to their length;
to wash the head is necessary not less than 1 time a week.
(h) The nails are cut once a week.
(i) External genital organs are washed with warm water; to girls with
the purpose of prevention of urogenital infections, the washing should be carried
out (Attention!) from front to back. (j) Hygienic baths — once a week; duration of a bath for 2
year old child is 8-10 minutes, after 2 years of age — 10-20 minutes.
2. Usually the clothes and the bed-sheets are changed once a week, iti < ii!K) of
necessity (the patient is in horizontal position, after vomiting etc.) it is •Mm the needed number
of times.
Changing clothes of the seriously ill patient should be carried out in the following order:
• First, the shirt is removed from the head.
• Then — from hands.
• The clean shirt is put on first on hands.
• Then — on the head and trunk.
In case of trauma or other damages to the arm, the sleeve at the beginning is removed
from the healthy arm, then —from the injured one; and the sleeve is put on the injured hand at
first, and then — on the healthy hand and arm.
In practice, the following rules and the order of two methods of change of the
bedding of the severely ill patient are applied:
(a) Perpendicularly,
• A bed sheet under the child is rolled up so that two bolsters are made: above the head
downwards approximately up to the waist and from below from the legs upwards up to
the waist.
• The formed double rolled sheet is removed.
• A clean bed sheet in the similar form of two rollers is laid under the waist of the child
across the trunk.
• One roller upwards is spread, to the head, another — downwards, to the legs of the
patient; then the bed sheet is straightened smoothly on the bed.
(b) Parallelly,
• The patient is put sideways on one side of the bed.
• On the other side of the bed, the dirty bed sheets are rolled lengthwise.
• On the same side of the bed, but without any dirty bed sheets a cleen sheet is put on
(Fig. — A).
• The patient is moved on to the clean sheet (Fig. — B).
• From the free side of the bed the dirty sheet is taken away, after that the clean one is
spread out (Fig. — C).
Methods of changing the bed sheets for the severely ill patient (in
parallel form)
ORGANIZATION OF WORK OF MEDICAL PERSONNEL IN CHILDREN'S
DEPARTMENT
Pediatricians, medical nurses and hospital cleaners work in children's department in our
country.
Work of medical nurses and hospital cleaners
Several medical nurses work in a children's department. They carry out different duties: a
senior medical nurse (= matron) supervises the work of all other nurses. Manipulation medical
nurse is responsible for giving injections, post medical nurse must distribute medicines to
patients, observe all patients, collect samples for analysis from patients, etc. Medical nurse
performs physiotherapeutic procedures, etc.
Usually in the afternoon, there are more nurses at work, than at night. If emergency
situations occur, which may arise anytime, a nurse must know and be able to perform all
recommendations of a doctor who treats or a doctor on call.
The basic duties of nurses
Participation during the process of admitting patients into hospital.
2.
Performing all recommendations assigned by a doctor (there is a special
prescription form where a doctor has to write all the necessary analysis and manipulations that
are to be done):
3.
Case history # 1337 at 29 May 2010 Full
name Andronjuk Sergeu
1.
Age 1 year
Body weight 10 kg
PRESCRIPTION FORM
Per os
#
Date
Mani
pulations
of
prescript
ion
Vitamin
1
1. C 0.025
t.i.d.[1]
Bronch
2
2. osan 5
gtt.
q.i.d*
29
.05
29
.05
Suprastinu
3
3. m 1/4 tab. .05
t.i.d.*
during
eating
29
Lin ex
4 1
4. caps, t.i.d. .05
a.c. * before
eating (open
29
of
withdra
wal
Date
of
prescript
ion
Cefazolinum
250
mg .05
b.i.d. IM
29
Acid urn
adenosintrip .05
hosphoricum
1% 0.5 ml
q.d.*IM
29
Phy
siotherapy,
of
Examinati
withdra
ons,
wal
Remedy
and
curative
gymnastics
General
blood test
Date of
prescript
ion
22
9.05
Urinalysis
22
9.05
Chest X-ray
22
9.05
ECG
33
0.05
and mix
with some
quantity of
sweet
water)
Consultation
of
0.05
cardiologist
33
Soda
inhalation #3 9.05
22
Chest UV
Radiation
33
0.05
(a) Distributing medicines to patients (in case the child is alone ,in a hospital, a
nurse should make sure that he/she takes the medicine on time and correctly).
(b) Dropping medicine into eyes, nose and ears.
(c) Carrying out different manipulations (e.g. intramuscular, intravenous
injections, infusion therapy, etc).
(d) Measuring weight arid height of children.
(e) Collecting samples for laboratory analysis from patients (blood, urine, stool,
nasal and oral swab, etc.), delivering them to the laboratory. When the analyses are
completed, it should be taken by the nurse from the laboratory and attached into the
case history.
(f) Taking general care of the patients and carrying out complicated methods of
treatment and examination of patient (feeding the child through a tube, catheterization
of urinary bladder,and gastrointestinal tract as well as indirect massage of heart, etc. —
all this we will study shortly).
(g) Transporting patients for radiography, spirography and other kinds of
specific examinations, physiotherapy, consultations with subject specialists, etc., and
timely submission of all the results after performed analyses and conclusions with
subject specialists to a doctor.
(h) Calling specialists for consultation from other departments of hospital.
(i) Carrying out hydrotherapy for patients and be present during the procedure,
if it is assigned by a doctor.
(j) Calling ambulance for transportation of patients.
4.
Permanent duties of a medical nurse that are carried out daily with no special
prescription made by doctor:
(a) Filling in medical documentation (except for case histories).
(b) Measuring patient's body temperature in the morning and in the evening,
sometimes the temperature should be taken every hour (if the patient is in severe
condition or undergoes infusion therapy) and sometimes even more often. The data are
to be put down into a Temperature sheet (Figs 64 — 66).
(c) In some cases, heart rate and blood pressure are measured (sometimes a
medical nurse puts down these data into the Temperature sheet of the case history —
see Fig. 66) measurement of respiration rate.
(d) Measuring weight and height of children once a week, according to a plan.
(e) Reporting every morning to the medical personnel of the department about
conditions of patients, especially those who are critically ill or newly hospitalized, and
about those whose condition unexpectedly got worse.
5.
Be present at general doctor's rounds, where all necessary information about the
condition of patients is given.
6.
Check if all necessities are delivered into department timely:
Medicines.
Medical tools and bandage materials.
Food for patients.
Sets of clean bed linen and underwear for patients.
7.
Stick to the following rules:
• Personal hygiene of patients.
• Order at the medical nurse's post.
• Storage of medical products which include:
2 groups of medical products that are to be stored in special metal boxes as safes with
inscriptions 'A' and 'B' or cabinet. Safe 'A' contains poisonous and narcotic
products. Safe 'B' is used for strong active remedies. Key to the safe should stay with
one of the officially appointed employees of the department (senior medical nurse, head
of the department) who bear the legal responsibilityfor preservation and distribution of
medicine. Inside the safe, there should be a list with names of medicines stored in the
safe and their daily and single pediatric doses. It is very important to have a list of
antidoses in the medical safe, for the purposes of treating children who might get
accidentally overdosed by various pharmaceuticals. All data about delivery and use of
these medicines should be timely put down into a special medical register.
Medical products with strong smell (e.g., liquid ammonia) and coloring solutions (e.g.,
iodine, methylenblau) are stored in a separate safe.
Other medical products are stored in regular cabinets. The medical nurse at the post looks
after them. The medicines in the safe are arranged in order convenience for usage. The
order of their arrangement may vary from department to department. Each shelf should
have a label with the name of the group of medicines on it — e.g., for internal or external
use, for injections, etc.; besides, it is convenient to divide them according to their form.
For example, internal medicines are produced as tablets, liquids, powders, etc.; it is
desirable to put the bigger bottles away from the smaller ones — it will enable you to
read the labels on bottles at once.
Additional rules of storing medicines:
It is necessary to keep a steady temperature and humidity of environment where the
medicines are kept (for example, some medical products — dry plasma, insulin, herbal
decoctions, etc. should be stored in a refrigerator at temperature from +2°C to +10°C,
fresh frozen plasma — in a freezer as a frozen substance), o There are medicines (for
example, iodine) which should be stored under certain illumination — for this purpose
they are stored in dark bottles and in dark places.
The medicine should not be used after the expiration date, which is always specified on the
label of the medicine. If there are visible changes in a normal look of a medicine
(dimness, flakes, change of color in liquid medicines; appearance of stains and change of
color in tablets; unusual smell of a medicine) is also an indication of the fact that
medicines should no longer be used, o Medical remedies should never be stored together
with disinfecting solutions.
7.
Teach children and their parents the following rules, if necessary:
•
Working hours of the hospital.
•
Getting food products from friends and storing them.
•
Taking medicines.
•
Personal hygiene.
•
Child care.
Supervising the work of a junior medical personnel:
• Controlling reception and distribution of food, and if necessary rendering
assistance in feeding patients who are in severe conditions.
• Supervising their main duty — i.e. keeping children's department of the hospital
clean and in order.
8.
The basic duties of a junior medical personnel:
• Damp cleaning in the medical institution (they should know the frequency of
cleaning and contents of the liquid used in different rooms).
•
Supervision of sanitary conditions of furniture in the ward, corridor, etc.
•
Sanitary processing of the patients, beginning with the reception.
•
Helping the child in observing the rules of personal hygiene (combing hair,
trimming nails, etc.).
•
Changing bed covers, bed sheets and patients' clothes.
•
Prevention of bedsores.
•
Necessary medical aid to a serious patient in micturition, defecation (for example,
to keep a bedpan).
•
Helping the nurse in some methods of inspection (collecting urine, stool; measuring
of weight and height of the child, etc.).
Work of the doctor-pediatrician in a hospital
In every children's department, there is a managing branch and attending physicians.
The basic duties of a doctor-pediatrician of the children's department include:
•
Admission of the patients (in case of the absence of a separate admitting
room).
•
Daily observation of the patients.
•
Daily filling up of the case history.
•
Daily viewing and additional filling of the list of medicines to be given).
•
Consultations with the patient's parents at their request during the whole
time of hospitalization, especially during discharge from the hospital (the explanation of
the child's condition, acquaintance with the results of inspections, advice, and
recommendations).
•
In the morning, obligatory presence at the briefing of medical personnels of
the department.
•
Simultaneously with the nurse — carrying out of some difficult manipulations (such as blood transfusion; intravenous introduction of plasma, contrast substances;
punctures, for example, pleural puncture, etc.).
•
On the day of discharging the child from the hospital, a 'Discharge form' is
written (the document in which the diagnosis, the prescribed examination, treatment and
recommendations are specified); it is given out to the parents or transferred to the
children's polyclinic.
Medical documentation of the children's department
The case history (= Medical record card of the hospitalized patient)
The average medical personnel in the case history fills the following suctions:
•
The passport section.
•
The result of examination on pediculosis.
•
The result of interrogation on possible infectious diseases (virus hepatitis,
tuberculosis).
•
•
A temperature sheet.
Once a week — the information about changing clothes and taking hygienic
baths.
The nurse should, at the required time, file in the the following documents InlQ the case
history :
•
Results from the laboratory and other (X-ray, ECG, etc.) kinds of
inspection.
•
The conclusion of specialists (ENT specialist, cardiologist, etc.), if the
consultation was carried out in other medical establishment (the case history of the child
cannot be taken out of the hospital).
The general rules of conducting and keeping of the case history:
•
The data about the condition of the patient should be recorded daily;
•
The observance of the form and order of the filling of different sections of
the document (we shall learn about this further on, in the course of propaedeutics)
•
After discharging the child from the hospital, the case history is transferred
to the archive, where it is stored for 25 years.
There is a special register which shows the patients' movement (the duty of a medical
personnel is to write the information into it). Every morning, all medical personnel gather in the
staff lounge: the persons who were on duty the previous night and those who must be on duty
during the new day. Usually such a gathering in our country is called a '5-minute' briefing. At
the beginning of this meeting, the duty doctor reports about the situation in a hospital:
•
Number of children in the department before the beginning of his/her duty
and number of children in the morning.
•
Number of children being admitted.
•
Number of patients discharged.
•
Number of children moved to some other hospital or ward.
•
Number of patients dead or has left the hospital unwarrantly.
•
Detailed information about the newly admitted children.
•
The condition of serious patients.
•
Possible reasons of deterioration of the condition of other children (rise in
temperature, problems in defecation, etc.) and maximum help rendered to him/her are
described.
Then, the nurse on duty reports on all the patients who had some increase in temperature,
or whose condition became worse, gives the list of those who did not hand over some analyses
with the indication of the reason, possible peculiarities of giving and taking medicines.
This information is especially necessary for the attending physician.
For example:
•
After the distribution of patients, the doctor starts the inspection of the child
whose situation is most severe (at the absence of such information, the severe patient may
be examined by the doctor too late, which may be very dangerous for his/her life, — for
example, at 12.00 — 1 p.m.).
•
The missing analyses should be prescribed repeatedly without any delay;
there are methods of the inspection, for example, swab culture on pathogenic flora, when
the result comes only within 2-3 days; i.e. at the absence of such information from the
nurse, the doctor finds out about the missing analysis only after some days.
•
In case of the unwarranted leaving of the sick child, the attending physician
should inform the local or family doctor about that immediately.
The nurses' register (or sheet) in different departments can have different names and
can be conducted unequally, but the most convenient way, — is_a document for duly
performance of all medical procedures specially for nurses. «unci this document has to be
filled in this register
In the register the attendant nurse on duty daily, sometimes 2 times a day, makes the
following extract of the sheet of the assignments (with mentioning the surname of the child):
•
Intramuscular injections (there may be a list according to the groups of
medicines, the time of introduction, the wards, etc.).
•
The list of necessary analyses.
•
Assignments for the inspection and the appropriate preparation for the
procedure.
•
The list of consultations, etc.
The register book of the department (Fig. 10) in which the information on
hospitalization of patients and their discharge is registered, has the following vertical columns:
Number.
Number of the case history.
Date of hospitalization.
Full name.
Age.
Address.
By whom he/she was refered from.
The diagnosis during hospitalisation.
The final diagnosis (at discharge).
Date of discharge.
When he/she is discharged to: home, transferred to some other department, fatal case.
Number of days in the department. Attention! The first and last days are considered
as 1 day: for example — if patient arrived on 2.02.2010, and was discharged on
7.02.2010, the number of days — 5.
The register-book of infectious patients in pediatrics is of special importance because
infectious diseases (measles, scarlet fever, pertussis /= whooping cough/, etc.) are most frequent
among children. The diseases of such character develop not later than 3 weeks after the contact
of the child with the infectious patient. Therefore, the patient who is hospitalised into the
children's department, for example, with pneumonia, but was in contact with the infected patient
7 days before, is dangerous for 2 more weeks. Probably, the infectious disease will be shown in
him/her, but may be, the child was not infected — it is not known by anybody. Such a child
cannot be put into a usual ward. Here, the doctor solves the problem individually: A patient
whose condition is not very severe can be treated at home, but a severe one — put into a
separate isolated disease will be shown in him/her, but may be, the child was not infected — II
is not known by anybody. Such a child cannot be put into a usual ward. Here, the doctor solves
the problem individually: A patient whose condition is not very severe can be treated at home,
but a severe one — put into a separate isolated ward and at presence of symptoms of an
infectious disease — directed to the infectious hospital. However, in each case, the information
on the patient like this is entered into the above-mentioned register-book of infectious patients
named above.
In the emergency messages book, the cases of emergency character are recorded (i.e.
demanding urgent finding out of the reason of the occurrence and prevention of spreading out
the pathology (infectious disease, poisoning, dangerous reaction to vaccination, medicines). The
information on these cases should be imported urgently to SES (sanitary-and-epidemiologic
station).
RULES OF DRUG ADMINISTRATION
There are some ways of the medicinal administration:
1. Enteral (=oral) — introduction of medicines through gastrointestinal It net (GIT):
♦ Peroral.
♦ Per rectum.
Parenteral — introduction of medicines by injection with skin damage:
Intradermal.
Subcutaneous.
Intramuscular.
Intravenous.
2. Through derma and mucous membranes without their damage:
♦ Manual application of the preparation on derma and mucous membranes.
♦ Electrophoresis.
♦ Inhalations.
2.
♦
♦
♦
♦
Enteral
Peroral (= Per os, p.o.) administration of medicines in pediatrics does not cause any
complication in children of older age. With this purpose, as well as in adult, medicines are used
in the form oftablets, capsules, granules, powders and liquids. At the time of prescribing
medicines, the doctor (or nurse) should explain the rules of taking the medicines:
© How many times a day, sometimes, it is necessary to specify the time of
reception (some medicines are given only in the morning or in the evening).
© Connection with meals— most medications are given after meal (for reduction of
their irritating influence on the mucous membrane of the stomach), some of them should
be used a.c. (i.e. before meals). Sometimes 45-50 minutes prior to a meal.
© Some peculiarities are possible. For example, Solutan should be taken with
some milk; as for Mucaltinum it is better to dissolve it in water and to add a little sugar.
Usually, the preparation is put on the root of the tongue, and then, the child takes some
drinks of water or other liquid tasty for him/her, simultaneously with which the medicine is
swallowed.
As for children of early age, especially during the first 2 years, it is difficult to give
them a medication per os. It is strictly not recommended to do it by force (!). Recently, this
problem has been solved by preparing medicines in the form of syrups. If syrup doesn't help,
then the medicine should be crumbled and mixed with a little amount sugar and water, or
dissolved in some tasty liquid.
The technique of giving medicine is: taking some medicine in a spoon, place the child in
almost a vertical position, close his/her nose and the child opens mouth in reply to this and
medicine is put in the mouth, then a favourite drink is given.
Per rectum (p.r.) is an administration of a suppository through the rectum.
The technique is as follows:
•
The child of an older age is made to lie sideways, with legs bent in knee
and hip joints, the nurse by one hand moves buttocks apart, with another hand she put the
suppository deep enough as the anus gets closed. Then for the prevention of slipping out
of the suppository, it is necessary to compress buttocks near the anus for some minutes.
•
The child of early age can be put on the back, with legs lifted upwards, and
further on, the technique of administration is similar to the above description.
Parenteral methods
For parenteral administration of medicine, a syringe is used, it consists of a cylinder, a
piston, the cone of which is located at the end of cylinder and u needle which is fixed on the
cone. Recollect!The end of the needle opposite lu the sharp end, is called as cannula — see.
a — the cylinder;
b _ the piston;
c — cannula of the needle'
d—the needle of 'butterfly'type
During last few years with the purpose of pi< mention of infectious diseases and
spreading gl AIDS plastic disposible syringes "Luer" are used.
Syringes are different depending on:
•
Volume and application — special for insulin and tuberculin, we use a 1 mL
syringe. (on the syringe, the measure of volume is indicated in mL and UA), widely used are —
on 2 mL, 5 mL, 10 mL, 20 mL, and more voluminous syringes (for example, 60 mL);
•
The location of the cone at the centre of the syringe or eccentric.
Needles also differ— in length, diameter, IIIo cut of angle at the end.
The general rules and order of parenteral administration:
(a) The place of injection depends on its kind; however, it is always that part of skin
which contains the least amount of nerve fibres and blood vessels (except for intravenous
injections).
(b) During injection, periosteum should not be damaged.
(c) For prevention of mistake, it is necessary to read the label on the ampule or the
bottle, to pay attention to the kind of medication, doze, expiry date.
(d) It is good to wash your hands; even at small injury of skin — to process it with
spirit; the presence of purulent damages on the skin is a contraindication for the injection; after
processing of hands do not touch anything.
(e) Put a needle on the syringe.
(f) Take some medicine into the syringe a little bit more than the necessary
volume (if the ampule or the bottle are placed above the needle — the liquid flows from
the top downwards, if it is under the needle — the liquid rises from below upwards).
(g) Always change a needle to a clean one.
(h) Lift up the needle, slightly let some liquid out so that air could go out from the
needle (thus, the superfluous amount of medicine will be removed).
(i) Before the first injections, it is necessary to prepare the child psychologically for this
procedure, not deceiving (!) him/her.
(j) The child should be kept into motionless position on the bed which relaxes the
muscles and promotes the best administration of the liquid; child should be held by mother.
(k) Process the place of the injection with 70% ethyl alcohol, ether, or 5% tincture of
iodine.
(I) Inject the needle approximately to 1/2-2/3 of its lengths — in case the cannula is
broken in the place of connection, it will be possible* to take it out without operation. If the
needle is put till cannula in that case, the broken part enters the tissues, that will demand surgical
intervention.
(m) The preparation is entered with the certain speed which depends on the following
factors:
• Less amount of liquid entered — demands a higher speed.
• Consistence of medicines — thicker medications are more slowly injected.
• Morbidity of a preparation — very painful medicine are not entered quickly, but also
not very slowly.
• The purpose of the procedure — here, the speed is specified by the doctor.
(n) The needle is taken away, and the place of the injection is wiped by spirit.
(o) Repeated injections are not done in the same place.
Intradermal injections (i.d.): From the name itself, it is clear that the medication is to be
administered in skin.
Features of the technique:
(a) The place of the injection is the internal surface of the forearm or external surface of
the shoulder.
(b) The needle and a syringe are of the least sizes, it is better to use the syringe with the
eccentric arrangement of the cone of a tip.
(c) The skin is processed with spirit or ether.
(d) The needle is placed with its cut directed upwards at an acute angle to the skin and
injection is done intradermally.
(e) If the medicine is entered correctly, a so-called symptom 'of lemon peer is
observed — the skin towers a little, a papule is formed, and many pits are formed (this reminds
the peel of lemon).
Mostly, such injections are done for the diagnostic purpose. For example, for
determination of the allergic reaction of an organism to antibiotic. Antibiotic In Injected into
the skin in the lower third of forearm in lower concentration (diluted). In 20 minutes, the size of
hyperemia around the place of the injection h visually evaluated. Normally, reddening is absent
or its diameter does not exceed 1 cm. If it is more — the preparation is contra-indicated for the
child.
In order determine to the condition of migration of water (and sodium) In tissues, i.e.
the hydrophilia of the tissues, the Mc Clure-Aldrich test is < ferried out (the U.S. doctor and
the biochemist of the 20th century): 0.2 mL of isotonic solution is injected with a thin syringe in
the region of the top half of luruarm. The time of resorption of the papule with lemon peel' is
taken into fi« count, which normally depends on age:
•
Under 1 year of age — 15-20 minutes
•
1-5 years — 20-30 minutes
•
Over 5 years — 40-60 minutes
I lie evaluation of the analysis:
(a) The time is lower than normal (i.e. accelerated resorption) — this is a sign of edema
of tissues of different character (cardiac, renal, etc.); if the edema of this kind can not be
observed, then, it is refered to as 'pitting' edema (see pg. 471), and can be established by
means of this method.
(b) The time is higher than normal (i.e. slow resorption) — this is a sign of dehydration
of the organism.
Subcutaneous injection (s.c.) is refered to, when the medicine is administered under the
skin.
Features of the technique:
(a) Places of the injection— top 14 of the shoulder, bottom of the forearm, stomach,
under the scapula, external surface of thigh.
(b) Needles and syringes — are both of different sizes. It is better to use syringes with
eccentric arrangement of the tip of the cone.
(c) The skin is processed with spirit or iodine.
(d) With the 1st and the 2nd fingers of one hand, skin and subcutaneous tissue are slightly
pinched (a fold is formed at this) and stretched upwards a little.
(e) The needle is placed at an acute angle to the skin and 1-2 cm of it is entered deep into
the skin.
(f) Draw the piston back and check the possibility that the needle has been injected in a
vessel — if blood is not present, then the medicine can be injected.
During intramuscular injection (i.m., IM) the medicine is injected into a muscle. It is
one of the most widespread parenteral method. The advantage of intramuscular injections in
comparison with subcutaneous is the quick absorption of the medicine due to lot of blood and
lymphatic vessels in muscles.
Features of the technique are as follows:
(a) The place of the injection is the top external quarter of the buttock and the top
anteroexternal quadrant of the thigh.
(b) Needles are long, of average diameter and syringes are of different volume.
(c) The skin is wiped with spirit or iodine.
(d) The needle is placed at an angle of 90° to the skin and is entered into, on a depth of
2-3 cm.
(e) A possible inadmissible introduction of the needle into a blood vessel is checked and
at the absence of blood the medicine is injected.
(f) For quick and better absorption of the preparation after injection, it is effective to
carry out massage in the place of the injection or put warm hot-water bottle.
Complications and necessary medical tactics
1.
Infiltration — hardening in the place of the injection — arises when a large
number of injections are done in closely located points, and also in case of the voilation of the
rules of aseptics.
It is determined by palpation, and the child often complain about pain in the place of
injection and a dangerous attribute is reddening of the skin in the place of infiltration.
Medical tactics:
Warming by means of the compress (semi-alcoholic or with heparin).
Iodine network[2] (Fig. 12)— a 'picture' in the form of grid is drawn at the place of the
injection with cotton bud moistened with 2% solution of iodine.
Ultra-Violet Radiation.
2.
Hemorrhage and bleeding arise mostly in case, when the end of a needle injures a
blood vessel. Probably, there may be a blood disease that onhance bleeding, which demands
special inspection of the child.
Medical tactics:
The nurse has to bandage this place pressing the bandage firm to the skin.
To inform the doctor immediately.
3.
Damage of nerve fibers occurs as a result of wrongful choice of place for
injection/The child experiences a sharp pain which feels like an electric '.liock. Further on, the
attributes of the voilation of functions of the injured nerve develops.
There may be a condition of anaphylactic shock.
The tactics of the nurse is to stop the injection and to call the doctor.
'Iodine network'in the top external quadrant of the right buttock
At the voilation of techniques of administration, the medicine can get into the
surrounding region — for example, embolism of the branches of pulmonary arteries with the
particles of oil solutions which have got into a vein during their intramuscular or subcutaneous
injection.
5.
Abscess — suppuration in the place of the injection— is the result of rude
voilation of the rules of asepsis, demands surgical treatment.
Medical terminology: the word Infusion' means parenteral administration of plenty of
liquid into a patient with diagnostic or medical purpose. Infusions can be intra-arterial,
intravenous, intraportal, subcutaneous, etc. Infusions are divided into stream (- set) and
droplet ones considering the administering speed.
Intravenous infusions (= injections) (i.v., IV) when medicines are injected into
peripheral veins, and this procedure is mostly applied at a serious condition of the child,
however they can be carried out during scheduled treatment.
A place of injection:
For children of the first years of life, veins in the area of radio-carpel joints are used
(this place is the best for being fixed in the immovable position during droplet administration),
less often — ulnar vessels and subcutaneous veins of the head as well as an area around the
ankle joint are used.
In older children injections are made into ulnar and radio-carpel regions, less often —
and talocrural joints.
Features of the technique of intravenous jet infusion as follows:
1. Needles— long, of a large diameter, with a short cut on the end, syringes — of big
diameter.
2. The skin is processed with spirit or p ether.
3. At the beginning, it is necessary to press the skin above the place of injection with i a
finger or a whole hand (the nurse-assistant I usually does that, or to put a tourniquet on).
4. The needle is placed at the surface of I a skin at a particular angle, along the
current of venous blood and pushed deep into untill piercing of one wall of vein [an
attribute of getting to a vein is the occurrence of blood in the cannula of the needle;
sometimes (at condensation of blood and dehydration of the organism) blood may not
appear]; In that case, it is possible to enter a sterile cotton strand — if the needle is in the
vein, the tip of the strand will redden.
Some nurses make injections at once, with a needle fixed to syringe; in such case the entrance in
a vein is determined by pulling the piston back where by blood will appear in the liquid in inside
the syringe.
A skilled nurse usually gets into a vein on first trial; otherwise, it is necessary, not to pull
the needle out of the skin, but to pull it back a little bit and try to enter the same or other vein; in
case of failure, the needle is drawn out and the place is pressed with a cotton tampon, moistened
in spirit; then some other place for i.v. injections is chosen.
5. As for stream infusions, usually, some medical products are injected by several
syringes which are serially inserted into the needle placed into a vein; as the medicines work
practically fast, they are injected slowly (!).
6. During one i.v. injection, not more than 50 mL can be entered.
7. After accurate removal of the needle from the skin, the place of the Injection is
processed with spirit, then for prevention of bleedings, a sterile pressing bandage is put
on.
In order to administer greater volume of medicines, intravenous droplet infusion are
applied when the liquid does not get into a vein, but the current of it is adjusted by drops which
can be seen.
At the beginning, a dripper system is prepared, the structure of which consists of:
1. A dripper in the form of plastic tube having the following parts:
♦ A special tap which can block a tube and, therefore, regulate the speed of
dripping medicines.
♦ The expanded part— of a dripper at the bottom of which a 'stagnant lake
of liquid' is formed, where the liquid from the upper part of the tube will drip with the
visual speed; the speed of the frequency of drops per minute, either its reduction or
increase is adjusted by the above mentioned special tap.
♦ The upper part of the tube ends in a needle which is inserted into a bottle
with medicinal liquid.
♦
At the bottom of the tube, there is a soft rubber site or closed 'hole' with a special filter,
with a cannula on its edge, which is put on a needle in the vein; through the rubber part, the
additional medical products are entered by jet infusion after closing the tap hence stopping
droplet introduction.
2. A stand on which the bottle with medicine (Fig. Intravenous infusion - A) is placed
upside down, for changing the pressure of liquid, the stand can be moved upwards or
downwards by a special regulator (Fig. Intravenous infusion - B).
For the appropriate movement of the liquid downwards, apart from the needle of a
dripper, one more needle should be inserted with its cannula open into the air, named among
medical personnels as 'air-needle' (Fig. Intravenous infusion - C).
Intravenous infusion
3. The needle in a vein — the older the child is, the wider and longer the needle is used.
In pediatrics, the so-called 'butterfly'-needles which are well fixed in immovable position
are very convenient vein, then, the needle is removed and a thin cannula remains in the vein (for
3-5 days), practically limiting the movement of the hand of the patient.
Sometimes, we can use a surgical method of inserting a catheter. So:
(a) The bottle with liquid is prepared, placed on a stand; the 'air-needle' is inserted.
(b) The dripper is connected to the bottle.
(c) Then, the tube is lifted upwards for a short time, in such a way that the
upper part of the dripper is below, then the liquid fills approximately the half of the
dripper. And the tube placed downwards at once — the liquid passes through the whole
tube up to the cannula. Special attention should be given, if air is present in the tube — it
should be removed (!).
(d) The tap is closed, and the lower end of the tube usually fixed to the stand for a short
time.
(e) The needle is entered into a vein.
(f) The tube is joined to a needle — for preventing the entrance of little
amount of air into a vein at this short moment, the liquid from the dripper should flow
and some amount of blood from the vein should come out.
(g) The frequency of drops is determined according to the prescription of the doctor —
from 10-12 up to 60 per minute.
(h) The needle is fixed — a sterile wadded tampon is put under it, and the needle is
fixed to the skin with an adhesive plaster.
(i) As infusion lasts for some hours, sometimes, during the day, the extremity is
fixed in an immovable position, it is especially important for children of an early age.
Usually, a splint (a hard plate) is placed under extremities, they are bandaged (do not
close the lower part of the tube and the needle!) and also fixed by a clip to the pillow or
mattress, rubber cord may be used if bandage is not available (above the cotton wool on
the hand), tie them to the frame of the bed. To little children, sedative medicines are
given, according to the doctor's prescription.
Attention! Nowadays, only the disposable dripper is used, which in case of long
infusion, should be replaced by a new dripper in 24 hours.
Complications of intravenous injections and medical tactics
2. Infiltration— it is formed, if the medicines enters surrounding tissues
Ihrough the injured vein or at wrong infusion, outside the vein. The tactics of the nurse is
using a warm compress.
3. Hemorrhage and bleeding — are formed at significant damage and puncture of a
blood vessel from two sides and at some blood diseases.
4. Air embolism — entering of some amount of air into the vein as a result of
professional mistakes, this demands urgent medical assistance. Air embolism due to a
considerable amount of air results in an irreversible condition of the patient which can lead to a
lethal outcome.
5. Phlebitis is an inflammation of the wails of vein into which the medicine is injected
by means of infusion.
Clinical attributes — pain and hyperemia of skin on a course of vein.
The principal causes are:
Infringement of the rules of sterility.
Long (more than 3 days) presence of the catheter in a vein.
Formation of blood clots in a vein may be in the following cases:
If necessary, the movement of liquid through a needle can be stopped for some
time. For this purpose, a mandrin is inserted into the needle. Cannula can be
closed with a special stopper, etc. However, a long delay of intravenous
infusion promotes the formation of blood clots.
For prophylaxtion of the thrombosis in veins (attention, which simultaneously
prevents the thrombosis of needles or catheter) a so-called 'heparin lock' can be
used — into a needle (catheter), 1 mL of the following contents are administered
— heparin and 0.85% solution of sodium chloride in the ratio of 1:9, after that,
the catheter (or the needle) is closed for the necessary time.
Very slow droplet infusion — 7-8 drops per minute.
The temperature of the medicinal liquid lower than body temperature of the
patient— is mostly observed at the infusion of plasma, albumin and blood, which
were stored in a refrigerator. Hence, such liquids before the infusion should be
warmed up to 37°C.
The treatment of phlebitis is to remove the needle, and put a compress with
heparin ointment along the vein.
6. Allergic reaction.
7. The infringement of the rules of administration, when the medication enters into
surrounding tissues — for example, if, during intravenous administration of calcium chloride, it
happens that CaCI2spills outside of vein, necrosis of the tissues will occur.
Measurement of respirations
Respirations are evaluated for (1) rate (number per minute), (2) rhythm (regular, irregular
or periodic), (3) depth (deep or shallow) and (4) quality (effortless, automatic, difficult,
laborated). A nurse also notes the character of breath sounds based on inspection without the aid
of auscultation, such as noisy, grunting, snoring, or heavy.
Examination of a pulse
A pulse is a rhythmic fluctuations of arteries walls, caused by emission of blood into
arterial bed and changes of blood pressure in it during systole and diastole. With each
contraction the left ventricle ejects a volume of blood (a stroke volume) into the aorta and then
into the arterial tree. A pressure wave moves rapidly through the arterial system where it can be
felt as the arterial pulse. The spreading of a pulse wave depends on the ability of arteries walls to
elastic extension and contraction.
P r o p e r t i e s o f p u l s e on artery: symmetry (synchronous or asynchronous), frequency
(accelerated, slowed, the pulse rate),
rhythm (rhythmic, arhythmic), tension (of
moderate tension,
dull,
soft),feeling (full,
empty),
size (high,
small,
thready), character (quick, slow), pulse deficiency (indicate the number of missing waves per
min).
Blood pressure measuring
Blood pressure in the arterial system varies with the cardiac cycle, reaching a systolic
peak and diastolic trough, the levels of which are measured by sphygmomanometer. The
difference between systolic and diastolic pressures is known as the pulse pressure.
Ambulatory blood pressure monitoring (ABPM) is a method of taking regular blood
pressure readings, usually over a 24-hour period, as patients conduct their normal activities. A
special, automatic blood pressure monitor is used, and patients are asked to keep a diary or log of
their activities during the day.
Ambulatory blood pressure monitoring is usually used when a physician suspects that a
patient is suffering from "white coat hypertension." This is a condition in which high
blood pressure occurs only in the physician’s office as a result of stress and anxiety.
However, there are a number of other situations that might cause a physician to
recommend ambulatory blood pressure monitoring. These include patients who do not respond to
medication and patients with symptoms such as fainting (syncope). In addition, ABPM has
been found to be a more accurate predictor of patients at high risk of a cardiac event than then
other blood pressure monitoring methods.
Ambulatory blood pressure monitoring is distinguished from home blood pressure
testing. Home monitoring systems are gaining in popularity. Relatively inexpensive, they allow
people to take their own blood pressure at various times throughout the day. Though this can
yield valuable information, there are several drawbacks when compared to ambulatory blood
pressure monitoring.
ABPM uses specialized equipment to measure blood pressure at regular intervals, 24
hours a day. This information is combined with a written log to aid in the diagnosis and/or
treatment of conditions related to blood pressure.
Ambulatory blood pressure monitoring (ABPM) is a method of taking regular blood
pressure readings over a 24- or 48-hour period. This is accomplished with a special device that
is worn at all times and measures blood pressure automatically, recording the readings.
Studies have shown that ABPM is a valuable tool in the diagnosis of several
conditions. It is also beneficial for adjusting doses of medication for high blood
pressure and even predicting cardiac events in certain patients.
Blood pressure is a measure of the force, or tension, of the blood against the walls of
the arteries. High blood pressure puts an added workload and strain on the heart, whereas low
blood pressure (hypotension) can lead to fainting (syncope). High blood pressure
(hypertension) is a very common disease in America. It is considered a major risk factor
for heart attacks and strokes.
Blood pressure is measured with the use of an arm cuff (sphygmomanometer) and
expressed as systolic pressure over diastolic pressure. Systolic pressure is the highest
level of the blood’s pressure within the artery walls and corresponds to the contraction of
the ventricle. Diastolic pressure is the lowest pressure at which blood stays within
the aorta. Both are measured in millimeters of mercury (mmHg).
In most cases, blood pressure is measured in a physician’s office. In recent years, blood
pressure measuring equipment has become available that allows people to measure their blood
pressure easily and affordably at home. In addition, monitoring equipment is often found in
public places, such as grocery stores and pharmacies. However, all of these approaches have
certain disadvantages that make ABPM an attractive option for some individuals. For example,
in the case of blood pressure measurements at a physician’s office, many people suffer from
“white coat hypertension,” or high blood pressure as a result of anxiety connected to the
blood pressure test itself. Similarly, the at-home tests and those completed out of a medical
setting may be inconsistent and unreliable.
By contrast, the ABPM measures blood pressure at regular intervals throughout the
monitoring period, including at night when the patient is asleep. It then records these
measurements. Coupled with an activity diary, the ABPM can give a physician a very accurate
picture of factors that may be affecting a patient’s blood pressure, such as exercise, eating,
medications and certain forms of heart disease.
This information is useful for a variety of reasons. For example, it may help the physician
adjust the dosages of antihypertensive medication. Many studies have shown that blood
pressure spikes in the morning, right around the time that 24–hour antihypertensives are at their
weakest. Thus, heart attacks and strokes may be more likely to occur in the morning. An
ABPM could help identify this situation, and the physician could adjust the patient’s medication
accordingly. Studies have also shown that ABPM may be a better predictor for certain cardiac
events than other methods of measuring blood pressure.
The special ABPM blood
pressure monitor is automatic, lightweight
(about 1 pound or less) and quiet. It consists of an arm cuff, a tiny computer and a small
compressor to inflate the arm cuff. The compressor and computer are generally worn on a belt
around the waist with a tube leading up to a cuff placed on the upper arm. The monitor is
programmed to automatically inflate the cuff at specific intervals during the ABPM period,
usually every 15 to 30 minutes. In cases of recurring fainting, measurements may be taken as
frequently as every seven to eight minutes.
The frequency of measurements may be programmed differently during the night to
minimize the disturbance to a patient’s sleep. The schedule also adjusts for the fact that changes
in blood pressure are less dramatic when the patient is at rest. There are two basic techniques that
can be used with the monitor cuff to read a patient’s blood pressure. Some monitors use one or
both of the following techniques:
CARE OF PATIENTS WITH CARDIOVASCULAR PATHOLOGY
Patients with diseases of the cardiovascular system complain of heart pain; palpitation and
intermissions in the heart's action, dyspnea, edema, a feeling of discomfort in the right
hypochondrium, headache, or fainting-fits.
Pain in the heart region is a serious complaint and its cause must always be revealed. Pain
can be the result of heart diseases (angina pectoris, myocardial infarction, myocarditis), of
pleurisy, intercostal neuralgia, injured ribs, etc. Cardiac pain varies in its character, duration,
localization and irradiation.
Retrosternal pain of a pressing character, arises during walking, exercise, nerve stress
associated with angina pectoris or myocardial infarction. It occurs due to insufficient myocardial
blood circulation. The nurse before the arrival of the physician must give first aid to such patient.
It is necessary:
To set or to lay down the patient, to ensure complete physical and mental rest.
To give the patient Nitroglycerinum ( 1 tablet under the tongue or 1-2 drops 1% of
Nitroglycerin Solution on sugar) or Validol tablets.
To put mustard plaster on the heart area.
Dyspnea is a most common complaint in circulatory insufficiency. The degree of dyspnea
varies. At first dyspnea develops during exercise when ascending stairs, and abates when the
exercise is discontinued. In cases of more pronounced circulatory insufficiency, dyspnea
develops during slight exercise, when the patient talks, and even when at complete rest.
The attack of dyspnea (cardiac asthma) is one with serious signs of an acute heart failure, which
requires emergency medical care. The attack of dyspnea occurs suddenly, respiration often becomes
increased often (3(M0 per minute), bubbling can be heard at a distance, there is a cough with a liquid pink
foamy sputum discharge. The nurse must:
- measure the arterial pressure;
- put the patient half sitting (in hypotension) or sedentary (in hypertension) position;
- give inhalation of oxygen, it must be moistened and passed through the ethanol alcohol
to depress formation of the gas bubbles in the respiratory tract. Dyspnea and asphyxia should
markedly decrease.
We can put a venous tourniquet on the extremity (thus a part of the blood is partially
deposited in the extremities, the volume of the circulating blood decreases and the work of a
left ventricle is facilitated).
It is possible to utilize rubber bandages or rubber tubes instead of a tourniquet. They are
applied simultaneously on three extremities: on legs the tourniquet is applied 15 cm below the
inguinal fold, on the arm — approximately 10 cm below the humeral joint. On one extremity
instead of a tourniquet, it is possible to apply a tonometer cuff forcing in air and simultaneously
utilizing it for the periodic control of the level of arterial pressure. Every 15-20 minutes one of
the tourniquets is taken out and it is applied on the free extremity.
Edema associated with heart diseases is another symptom of circulatory insufficiency. If
edema is pronounced, the liquid is collected into the body cavities (abdominal, pleural,
pericardial).
Proper care of patients with cardiovascular insufficiency is an important factor in their
treatment. It is necessary that the air in the ward should be fresh, of normal temperature and
humidity. For patients with pronounced circulatory insufficiency, prolonged bed-rest is often
prescribed, and the bed linen should therefore be free from knots that might press on the patient's
body, to prevent the formation of bedsores. It should be remembered that prolonged bed-rest may
cause blood congestion in the lungs and pneumonia.
A position of the patient in bed must be with the raised head. This reduces dyspnea and
facilitates the respiration of the patient. It is necessary to control the daily urine and the amount
of liquid that is drinked and injected parenterally. The daily urine should not be less than 70-80%
of the consumed liquids. If the patient discharges less urine than he consumes (negative diuresis)
it means that a part of liquid is deposited in the organism, the edemas are enlarged and the liquid
is collected in cavities. If the amount of urine discharged per day is equal to the total amount
of consumed liquid, this means positive diuresis. Edemas and the amount of liquid in the cavities
will reduce.
In chronic heart failure the patients as a rule have got the expressed trophic changes of the
skin, especially marked, in the field of edemas: on legs, the loin, scapulas, due to affection of
the skin nutrition. Decubituses easily occur in these places.
The patient should follow a light diet, high caloric, with inclusion of a cellulose with a
large amount of vitamins and appreciable restriction of salt and liquids.
It is necessary to stimulate the work of the intestine: in case of constipations, if it is
necessary to give the patient a hypertonic or oil enema (clyster).
A headache can be a sign of many diseases, requiring emergency aid. Pulsating, pressing
pain , frequently localized in the area of back of the head is one of the signs of hypertension.
In this case it is necessary:
To lay the patient in bed with a raised head of the bed , ensuring complete physical and
mental rest.
To measure arterial pressure.
To air the room.
To put mustard plasters on the back of the head and calf muscle or the hot foot baths,
warm baths for the arms can be used to redistribute circulation. It is possible to do a bloodletting or to put a medical leeches.
Сhildren’s temperature measuring
Body temperature changes during the day. Usually it is higher in the afternoon than in the early
morning. If a child is very active, his/her temperature may be higher than normal. Fever is a
protection for the body. A rise in body temperature above normal (usually 36.6° C=98.6° F
axillary temperature) lets you know that there may be an infection somewhere in the body. Fever
also helps the body fight the infection. Someone has a fever if the body temperature is higher
than 37° C=100° F (oral) or 37.5° C=100.4° F (rectal temperature).
Where to Take the Temperature:
Temperatures measured rectally are the most accurate. Temperatures measured orally, by
electronic pacifier, or by ear canal are also accurate if done properly. Temperatures measured in
the armpit are the least accurate, but they are better than no measurement.
Age less than 3 months old (90 days old):
An armpit temperature is preferred for reasons of safety and is adequate for screening. If the
armpit temperature is above 99°F (37.2°C), check it with a rectal temperature. The reason you
need to take a rectal temperature for young infants is that if they have a true fever, they need to
be evaluated immediately.
Age less than 4 or 5 years old:
A rectal or electronic pacifier temperature is preferred. An axillary (armpit) temperature is
adequate for screening if it is taken correctly. An ear thermometer can be used after 6 months
old.
Age older than 4 or 5 years old:
Take the temperature orally (by mouth) or by ear thermometer.
How To Read A Thermometer:
There are two types of glass thermometers, oral and rectal. The only difference between the two
kinds is the shape of the silver tip. A rectal thermometer has a short rounded tip. It is shaped this
way to prevent any damage to the rectum. The oral thermometer has a longer slender tip. Either
can be used for an axillary temperature.
While holding the clear (or white) end of the thermometer at eye level, slowly turn the
thermometer until you can see the silver line (mercury) (Fig. 1). The lower numbers on the
thermometer will be on the left. The amount the mercury moves from left to right will depend on
your child's temperature. The highest number that the silver line reaches is the right temperature.
Before using the thermometer, make sure it reads 96° F or less. If not, while holding the clear
end, shake the thermometer sharply above a soft surface, such as a bed or sofa, in case it should
fall. Look at the reading again. If it is below 35.5° C=96° F, measure the temperature. If not,
repeat the shaking until the reading is below 35.5° C=96° F.
Equipment: Glass thermometer, clock/watch.
How To Measure Axillary Temperature
Measuring temperature in the axilla (armpit) is the safest way to check if your child has a fever.
Tell the child that you are going to measure his temperature.
Wash your hands.
Have the thermometer and watch ready.
Look at the thermometer to make sure it is reading below 35.5° C=96° F.
Place the thermometer under the child's arm. The thermometer's silver
tip should rest in the center of your child's armpit.
Hold the child's arm firmly against his body.
Look at the time.
The thermometer must remain in place for 7 to 10 minutes. This may seem like a long time. To
help make the time seem to go faster, read a
story or watch television with the child. Make sure you hold the thermometer securely.
Remove the thermometer and read.
Praise the child for his help.
Write down the thermometer reading and the time of day.
How To Measure Oral Temperatures
By 5 or 6 years of age, a child can understand how to safely hold the thermometer in his mouth.
If the child has had something to eat or drink, wait 15 minutes before you measure an oral temperature.
Tell the child why you want to measure his temperature.
Wash your hands.
Have the thermometer and watch ready.
Look at the thermometer to make sure it is reading less than 35.5° C=96°F.
Place the thermometer in the child's mouth, far back under the tongue. Tell him to breathe
through the nose and not to talk.
Make sure the child does not bite the thermometer.
Look at the time.
Tell the child that the thermometer must stay in place for 2 to 3 minutes. Read a story or watch
TV with him.
Remove the thermometer and read.
Praise the child for his help.
Write down the thermometer reading and the time of day.
How To Measure Rectal Temperatures
Note that rectal temperatures should not be taken if the child has diarrhea or is less than 1 year
old. In taking a child's temperature, use the following procedure:
Tell the child that you are going to measure his temperature.
Wash your hands.
Have the thermometer and watch ready (and a clean diaper if needed).
Look at the thermometer to make sure it is reading less than 35.5° C=96°F.
Measure 2.5 cm (1 inch) on the thermometer.
Place the child on his stomach (Fig. 3), on one side with the upper leg bent, or on back with both
legs up.
Dip the thermometer's silver tip in a lubricant such as petroleum jelly (Vaseline).
Place the silver end of the thermometer into the child's anus.
Do not insert the thermometer any further than 2.5 cm (1 inch).
Look at the time.
Hold the thermometer in place for 2 to 3 minutes. Always hold the child so that he cannot twist
around.
Remove the thermometer and read.
Praise the child for his help.
Wash your hands with soap and water Count to 10 while washing, then rinse with clear water
and dry.
Write down the thermometer reading and the time of day.
How to Take a Digital Electronic Pacifier Temperature
Have your child suck on the pacifier until it reaches a steady state, and you hear a beep.
This usually takes 3 to 4 minutes.
Your child has a fever if the pacifier temperature is above 100°F (37.8°C)
Nursing care of the child with elevated body temperature.
Body temperature changes during the day. Usually body temperature is higher in the afternoon
than in the early morning. If a child is very active, his/her temperature may be higher than
normal. Fever is a protection for the body. A rise in body temperature above normal (usually
36.6° C or 98.6° F) lets you know that there may be an infection somewhere in the body. Fever
also helps the body fight the infection. Someone has a fever if the body temperature is higher
than 37° C (100° F) (oral or axillary temperature) or 37.5° C or 100.4° F (rectal temperature).
Clinical signs of increased temperature:
flushed skin, increased respiration and heart rates,
malaise,
“glassy look” to eyes.
You should measure a child's temperature:
When he feels warm to your touch.
When the child is not acting like himself.
Before calling your health professional to say that the child is sick.
Call your health professional as soon as possible if:
(1) the child has a temperature higher than 39.5° C(105° F)
(2) a fever (oral or axillary temperature above 37° C(100° F) or 37.5° C (100.4° F) rectally) is
present and the child:
Is less than 2 months of age.
Has a stiff neck, severe headache, stomach pain, persistent vomiting, purple spots on his skin, or
earache with the temperature.
Has a serious illness in addition to the fever.
Is confused or delirious.
Has had a convulsion.
Has trouble breathing after you have cleaned his nose.
Is hard to awaken.
Seems sicker than you would expect.
Cannot be comforted.
Has a temperature that continues to rise after medicine has been given.
Call your health professional during of-ice hours if:
The temperature is between 104° F and 105° F, especially if the child is less than 2 years old.
Burning or pain with urination.
The fever has been present for more than 72 hours.
The fever has been present for more than 24 hours without a known cause.
The fever went away for more than 24 hours, then returned.
The child has a history of febrile seizures.
You have some questions.
Table shows the average normal temperature standards for well adults at various bodv sites.
Oral
Rectal
Axillary
Esophageal
37°C
37.5°C
36.5°C
37.3°C
98.6°F
99.5°F
97.6°F
99.2°F
Not only elevated temperature itself, but also its circadian variations are very importamt for
diagnosing the diseases. Variations of temperature during the day determine the type of fever.
The following main types of fever are differentiated.
1. Constant fever (febris continua) — within day the difference between morning and evening
temperature does not exceed 1°C, morning temperature smaller than evening one. It is observed
in patients with acute lobar pneumonia or II stage typhoid fever.
2. Remittent fever (febris remittems): the daily fluctuations of the temperature exceeds 1 C and
the morning's lowest temperature being over 37 °C, the morning temperature smaller than
evening one. It often occurs in tuberculosis, purulent diseases, III stage typhoid fever and lobular
pneumonia.
3. Intermittemt fever (febris intermittens), the daily fluctuations of the temperature exceed 1 °C,
morning temperature smaller than evening one. The body temperature alternates
regularly between a period of fever and a period of norma] temperature. It occurs in malaria.
4. Hectic fever (febris hectica): the temperature rises sharply (by 2 ° — 4 C) and drops to normal
and subnormal level, that is often accompanied by excessive sweating, morning temperature
smaller than evening one. It usually occurs in grave pulmonary tuberculosis, suppuration, sepsis
and lymphogranulomatosis.
5. Inverse fever (febris inversus) is type of fever, when morning temperature is higher than
evening. It sometimes occurs in sepsis, tuberculosis and brucellosis.
6. Irregular fever (febris irregularis) — the fever, when cicardian variations are varied and
irregular. It often occurs in rheumatism, endocarditis, sepsis, tuberculosis.
According to the temperature curve recurrent (relapsing) and undulate (Malta) fever are
distinguished.
7. Reccurent fever (febris reccurens) — is characterized by alternation of fever and afebrile
periods. It occurs in relapsing fever.
8, Undulant fever (febris undulans) — is characterized by periodic elevation of the temperature
followed by its drop. It often occurs in brucellosis and lymphogranulomatosis.
Care plan
The most important thing to remember is not to bundle up the child with extra clothes and
blankets. Dress him in light clothing. This will help cool him by letting air circulate and heat
leave the body.
When a fever is present, it increases the amount of liquid that is needed by the body. It is
important to encourage the sick child to drink fluids. Some things that may help encourage him
to drink are:
straws,
small cups instead of a big glass,
popsicles,
jello,
soft drinks with the fizz removed (stale). The carbonation can be removed by leaving the soft
drink uncovered, by warming the soda in a microwave or on a stove, or by stirring in ½ teaspoon
sugar.
Medicines should not be used routinely to lower the temperature. If the child is uncomfortable
and the fever needs to be treated with more than light clothes and increasing fluids, then drugs
can be used.(Acetaminophen brand names: Panadol, Tylenol; tablets: Chewable Anacin 3,
Chewable Tylenol, Chewable Junior Strength Tylenol).
Duties of nurses during feeding children of different ages.
BREAST-FEEDING
Normal Infant Nutrition
Advantages of breast feeding:
Child
Mother
Family
Prophylactic of
Prevention of postEconomic advantages
infectious and allergic illnesses pregnancy complications
Prophylactic of
illnesses of digestive and
Healthy child
Prevention of unwanted
endocrine systems
pregnancy during the 4-6 month
after the birth of the child
Provision of
Preservation of reproductive
physiologic development
health
High index of
intellectual development
Healthy society
Prophylactic of cancer
illnesses
Psychoemotional unity
Tips of breastfeeding:
Some expectant mothers are concerned that breastfeeding will be too hard to learn. The most
important skill for them to master is getting the baby onto the breast correctly.
There are three basic breastfeeding positions.
1. Cradle — Hold your baby in one arm, with its head resting in the bend of your elbow. The
baby’s lower arm is tucked out of the way. Its mouth is close to your breast and the two of you
are tummy to tummy. This is the most frequently used position. This position can be used when
you are sitting up in bed with pillows supporting your back or sitting in a chair.
2. Lying down — Lie on your side with your baby also lying on his/her side. You are tummy to
tummy with the baby’s mouth close to your breast. This position is ideal when you are lying in
bed.
3. Football — Place the baby on a pillow at your side. Support its head with your hand. The
baby’s mouth should be in front of your breast. This position is good for smaller or premature
babies who might have trouble nursing.
“Latching on” is the expression breastfeeding experts use to describe how a baby grasps the
mother’s nipple with his/her mouth. It is a skill that a baby must learn with a little help from
his/her mother.
First, get the baby to “root” for breast. Rooting is a natural reflex for babies. The baby’s mouth
opens wide and its head moves quickly from side to side, searching for the nipple. To start a
baby rooting, lightly touch a nipple to the baby’s lower lip. When the baby’s mouth is wide
open, lift a breast to its mouth. At the same time, pull the baby close, so he/she can latch onto
mother’s nipple.
Proper latching onto nipple.
nipple.
•
•
•
•
•
•
Wrong latching onto
Other advantages of breast milk versus cow’s milk:
Breast milk is available all the time and is practically free from pathogenic bacteria.
It needs no time for preparation
It is available at the optimum temperature.
It contains antibodies as IgG and IgA and protects against certain infections such
as E.Coli, cholera, polio, tetanus, measles etc. IgA antibodies prevent the microorganisms
to adhere the intestinal mucosa and provide local GIT immunity.
β-lactose is called Bifidus factor, which promotes the growth of lactobacillus and helps
to lower the gut pH, thus inhibiting the growth of E.Coli and yeasts.
Breast milk contains lactoferrin (an iron-binding whey protein), which inhibits bacterial
growth by depriving them of iron, which is necessary for growth.
•
•
•
•
•
•
Breast milk contains cystine and tyrosine, which are not synthesized by infants but they
are essential for proper growth and development.
Breast milk contains taurine that is synthesized in inadequate amounts in infants. It is
important for normal differentiation of CNS.
Breast milk contains nonspecific factors of
immune difence: lisozyme, macrofagocytes, neutrofiles, lymphocytes, complement
system.
There are 5 times more essential fatty acids
(polyunsaturated: arachidonic, docosahexacnoic, linoleic, and α-linolenic) in breasts milk
than in cow’s milk.
Breast milk contains ferments (lipase, lactase) and mothers hormones.
Breast milk is ‘species specific’ and therefore allergy to breast milk is rare.
Dilution of Cow’s Milk:
Child’s Age
Cow’s Milk
Water
First 10 days
1 part
2 parts
10 to 20 days
1 part
1 part
Up to 2 mo
2 parts
1 part
If dilution of cow’s milk is required, add 1 TSF of sugar to each ounce of water (5 %) –
isocaloric formula)
•
Advances in nutritional modifications of infant formulas
Proteins: their amount is adopted to the needs of infant’s organism. Almoust all formulas
contain whey:casein ratio as 60:40 and adopted amino acid content.
Amino acid Breast Cow’s “Vitalact” “Similac”
milk
milk
•
•
•
Valine
8.2 %
6.6
4.6 %
6.8 %
Lysine
10.95
7.8
9.7 %
8.4 %
Trypto-phan
2.29
1.4
2.4 %
1.4 %
Fats: long-chain polyunsaturated fatty acids are added in amounts similar to those in
human milk. Infants fed these formulas or human milk have higher tissue concentrations
of long-chain polyunsaturated fatty acids and reportedly have better visual acuity than do
infants fed nonsupplemented formulas.
Carbohydrates: they are presented by β-lactose, sucrose, dextrin-maltose, which improve
the growth of Bifidum-bacteria. The total quantity of carbohydrates in formulas is 7.5 %
Nucleotides and their related products play key roles in many biological processes.
Although nucleotides can be synthesized endogenously, they are considered
"conditionally essential." Nucleotide concentrations in human milk are higher than
in unsupplemented cow milk-based formulas, and studies in animals and human infants
•
•
suggest that dietary nucleotides play a role in the development of the gastrointestinal and
immune systems
Medicines that should be avoided with nursing mothers
Medicines that should be avoided with nursing mothers
Medicines that should be avoided with nursing mothers
No
Drug
.
Reported sign or symptom in infant or effect on lactation
Aspirin (salicylates) Metabolic acidosis (dose related); may affect platelet function;
hemorrhagic rash
Drowsiness, irritability, refusal to feed, high-pitched cry, neck
2. Clemastine
stiffness
Sedation; infantile spasms after weaning from milk
3. Phenobarbital
containingphenolbarbitol, methemoglobinemia
1.
4. Primidone
5. Sulfasalazine
Sedation; feeding problems
Bloody diarrhea
Drugs of abuse that are contraindicated during breast-feeding
No
Drug
.
1.
•
Irritability, poor sleep pattern
Cocaine
Cocaine intoxication
3.
Heroin
Irritability, Heroin intoxication
5.
•
e
2.
4.
•
Amphetamin
Reported sign or symptom in infant or effect on lactation
Nicotine
(smoking)
Phencyclidine
Shock, vomiting, diarrhea, rapid heart rate, restlessness;
decreased milk production
Potent hallucinogen
Other reasons why a mother may not breastfeed her baby:
Working outside the home makes it more difficult to breastfeed exclusively, especially if
there is no support at her workplace for her to either bring her baby or to express and
store her milk.
Choosing not to breastfeed for personal reasons, either from the birth of the baby or after
breastfeeding for a short while, is a mother's prerogative.
Recommendations for Working Women:
The mother who goes back to work can usually continue breast-feeding without
problems. The milk supply adjusts itself to the demand. If the mother is working at least
8 hours a day, it is sometimes prudent to pump the breasts once during her work day in
order to stay comfortable and maintain a good milk supply. Each woman is different in
what is required to maintain a supply. Some women can work for a long time without
•
•
•
•
•
•
•
•
•
pumping and without compromising the supply. Others have a supply that is more
responsive to decreased feeds. A woman will rarely “dry up” because she has returned to
work.
Working mothers, however, can easily breast-feed part-time and formula-feed part-time.
Breast pumps and storage of milk
Hand expression is superior if the mother can learn the technique.
Several pumps are available if the mother is unable to express by hand.
It is good if the woman can borrow a pump from a friend before she decides which pump
to purchase. Another alternative is to rent an electric pump.
Milk should be stored in clean containers and immediately refrigerated or frozen.
– If refrigerated, it will stay good for 48 hours.
– If frozen at 0°F, it wiil keep for months.
Recommendations for mother’s diet:
To drink approximately 64 oz of fluids per day.
The nursing mother requires an additional 500 calories and 20-30 g of protein a day.
She has to take her prenatal vitamins with iron.
The mother need not to avoid certain foods unless she observes consistent increased
fussiness in the baby in association with the mother ingestion such foods.
Foods commonly incriminated:
Garlic
Onions
Cabbage
Chocolate
Great quantities of caffeine.
Nursing mother may drink small amounts of alcohol: a glass of sherry or wine may be
beneficial in late afternoon if she is having let-down reflex problems.
•
•
•
•
•
Length of Feeding - 10 - 15 minutes on each breast. Longer amounts of time will lead to
sore nipples, tired baby, and frustration for mom and baby.
Number of daily feedings:
First 2 months of life: 7 feedings per day every 3 hours with night break in 6 hrs.
3-5 months of life: 6 feedings per day every 3,5 hours with night break in 6,5 hrs.
After 6 months: 5 feedings per day every 4 hours with night break in 8 hrs.
Food stuffs
WHO recommended plan of weaning in breast feeding
Time of
Age (in months) depending volume of food
giving
6
7
8
9
10-12
Juice (fruit,
vegetable), ml
6
30-50
50-70
50-70
80
100
Fruit puree, ml
6
40-50
50-70
50-70
80
90-100
Vegetable
puree,g
6
50-150
150
170
180
200
Groats, g
(porridge, rice,
buckwheat)
Cereals, g
(semolina,
barley, corn)
Yoghurt, kefir
ml
6-7
5-50
50-100
150
180
200
7-8
5-50
50-100
150
180
200
8-9
-
-
10-50
50-150
150-200
Soft cheese, g
6,5-7,5
5-25
10-30
30
30
50
Yolk
7,0-7,5
-
1/8-1/4
¼-½
¼-½
½-3/4
Meat puree, g
6,5-7,0
5-30
30
50
50
50-60
Fish puree, g
9-10
-
-
10-20
30-50
50-60
Vegetable oil
6
½ tsp
½ tsp.
1 tsp
1 tsp
1 tsp
Butter
6-7
½ tsp
½ tsp
1 tsp
1 tsp
1 tsp
Bread, g
8-9
-
-
5
5
10
IF PROBLEMS ARISE...
Difficulties which arise in the early weeks of breastfeeding can seem overwhelming to th
e mother who is exhausted from lack of sleep or experiencing pain. Some women question their
ability tocontinue nursing during this time. It is at this point that the support and encouragement
of the father can contribute greatly to the success of breastfeeding. Here are some common conce
rns and problems youcan help to offset:
Nutrition During Lactation:
Breastfeeding women do not need to eat any special diet. They should eat a regular
healthy diet. Eat a variety of healthy foods from the food pyramid. Include three servings from
the milk group, two servings from the fruit group and and three servings from the vegetable
group daily.
A breastfeeding woman may be more hungry than usual and she should listen to her body
and add additional servings from the fruit, vegetable and bread and cereal groups.
It is nessessary to drink to thirst. Many women find that they are often thirsty while
lactating. They must try to minimize caffeine containing beverages, because the caffeine will
pass into the breastmilk. Water, milk and fruit juices are excellent choices for the new mother.
It is nessessary to minimize the amount of empty calorie foods consumed, so that there is
more appetite for nutrient rich foods. No one food or food group should be eliminated from the
diet unless a specific infant has a very clear reaction to a specific food.
Rapid weight loss through diet or medication should not be attempted during lactation.
Common Problems During BreastFeeding
Although breastfeeding is the recommended method of feeding infants, it is not without
complications or occasional discomforts for the mother. By being aware of these common
problems, the health care professional can offer advice to mothers to help alleviate potential
difficulties. As a general rule, breastfeeding should be continued through most illnesses,
including periods of diarrhea. Some of the most common problems are listed below.
Sore Nipples: Most women experience sore nipples at some period during their
breastfeeding course, especially during the first 2 weeks postpartum.13 Frequent, short nursings,
repositioning the infant at the breast, applying cold packs or heat to breasts, avoiding irritating
soaps or lotions on nipples, air-drying nipples after nursing, exposing nipples to direct sunlight
or 60 watt bulb for 15-20 minutes three or four times per day, applying vitamin E squeezed from
capsules or ointment such as vitamin A & D, pure lanolin or Masse¢ cream to nipples, and
avoiding the use of nipple shields may help ease the pain of sore nipples.13, Occasionally, sore
nipples are caused by a Candida albicans. The breasts may not appear to have a fungal infection,
but cultures of nipple surfaces will be positive for Candida albicans. 11Women often report
shooting pains at the end of a nursing when sore nipples are caused by a fungal infection. 11
Prescription for Sore nipples:
Nipple soreness in the first few days of breastfeeding is most often caused by poor
positioning. Review these relief measures and refer new mother to registered nurses and lactation
consultants at a local maternity hospital if she needs further help. Many Hospitals Have "warmlines" or other 24 hour telephone services for new parents.
Check for proper positioning. Baby should be latching onto at least 3/4" of the areola, not
just the nipple
Break suction at end of feeding by inserting a finger or pulling gently down on baby's
chin
Offer least sore side first
Alternate nursing positions
Express some milk and let it dry on nipple
Air dry nipples 10-20 minutes after each nursing; mother can also apply warm, dry heat
using an electric lamp or hair dryer on low setting
Apply steeped, cooled regular teabags to nipples for 10 minutes after feedings
If breasts are overfull, express enough milk to make areola soft before nursing
Avoid plastic in breast pads; change pads frequently
Treat baby and mom for thrush if this is causative factor (both may not have symptoms,
but both need treatment)
Avoid tight fitting bras and clothing
Use soothing techniques other than nursing to calm infant
Engorgement: The first engorgement caused by increased blood flow and filling of the
breasts will occur on the third or fourth day postpartum, usually without discomfort.11 However,
some women experience rapid filling of the breasts causing increased engorgement and
discomfort. Blocked mammary ducts may also be a cause of pain. Frequent nursings, breast
massages once or twice a day or before feedings, hot or cold packs, wearing a firm bra for
support and avoiding the use of nipple shields can help alleviate some of the discomforts of
engorgement. 27 The best way to prevent engorgement is to begin breastfeeding as soon as
possible after birth followed by subsequent frequent nursings. 27
Mastitis: Mastitis is a breast infection causing chills, fever, flu-like symptoms, redness
and breast sensitivity. It may be a complication of a clogged mammary duct or caused by an
infection carried from the baby. 11, 27 The primary goal in treating mastitis is emptying the
infected breast. Healthy infants are not at risk for developing illnesses by nursing during mastitis
and frequent nursing is actually encouraged.11, 27 If a mother develops symptoms of mastitis her
physician should be notified. Antibiotics or pain relievers that are safe during breastfeeding are
often prescribed. If mastitis goes untreated, an abscess could develop. Applying heat (not cold)
to the breast, drinking plenty of fluids and adequate rest are advocated to aid in the healing
process.11
Jaundice: The onset of breastmilk jaundice is typically at 1-2 weeks of life and occurs in
about 1% of the population of breastfeeding newborns.12 It is apparently caused by the presence
of a substance in the breastmilk that enhances red cell hemolysis or alters liver function.27 It is
rarely necessary to stop breastfeeding. Mothers should be encouraged to breastfeed 10-12 times
per day as frequent nursingsare inversely correlated with serum bilirubin levels. 11, 12
Poor Milk Supply: Poor milk supply can be a cause of failure to thrive in breastfeeding
infants. Maternal causes of poor milk supply are hypothyroidism, excessive antihistamine use,
oral contraceptive use, excessive caffeine intake, illness, poor diet, decreased fluid intake,
infrequent nursings or fatigue.12 Correction of any of these causes may improve milk supply.
Nipple Confusion: Infants who are breastfeed may refuse to take a bottle as the weaning
of breastfeeding occurs. The same musculature is necessary to suck from either a breast or bottle,
however, the spatial arrangement of the tongue and nipple differs from the two modes of
feeding.11 If the mother plans to feed formula from a bottle at anytime during the first year of
life, advise her to offer a bottle during the first 2-4 weeks of life and then offer one bottle per
week thereafter to decrease the incidence of nipple confusion. The bottle feedings can be given
using expressed breastmilk.11, 12
BOTTLE FEEDING
How to prepare baby’s formula:
Wash your hands before you begin.
Wash all bottle feeding equipment in hot, soapy water. Rinse well with hot water.
Sterilize bottle feeding equipment for the first three or four months of baby’s life. To sterilize,
cover items completely with water and boil for five minutes. Cool and remove from water with
sterile tongs.
The water for formula should be boiled for five minutes then cooled. Use safe drinking water to
prepare the formula.
Mix formula according to package directions. Fill the sterilized bottles. You may prepare up to a
24-hour supply of infant formula at one time.
Store the prepared formula in the refrigerator. When away from home, store it with an ice pack
in a cooler. Formula should never be left at room temperature for longer than one hour.
How to warm baby’s formula:
Place the bottle in a container of warm water or hold it under warm running tap water. Gently
shake the bottle for even warming.
Check the temperature of the formula before feeding a baby. Put a few drops on the inside of
your wrist. It should feel slightly cool.
Caution: Never microwave formula. Microwaves heat unevenly and a baby’s mouth could be
burned.
Caution: Never prop a bottle. It is a choking hazard and can cause baby bottle tooth decay.
Burping:
Wait until baby stops drinking.
Gently rub or pat baby’s back.
Rest baby on your shoulder or lap.
Burping the child.
Feeding Solid Foods
Feeding Techniques:
Food is for nutrition, not for rewards, bribing or punishment
Start with small portions
Introduce one new food item at a time
Wait until baby gives permission to put food in his/her mouth
Use high chair if baby can sit
Use appropriate utensils
Reduce distractions
Menus for toddlers (1-3 years)
“What and how much should I feed my toddler?”, is a question that is often asked. Dietician Dr Ingrid
van Heerden gives useful advice to parents.
Rule of thumb
The basic rule of thumb which can be applied to the dietary intake of toddlers from the age of one to
three years, is as follows:
1 Tablespoon of each food for every year of life
Thus a one-year-old child would be given one tablespoon at a time of cereal, pureed fruit, cooked
meat, cooked vegetable, and one egg, and milk and dairy products in portions of ½ a cup at a time.
A two-year-old child would be given two tablespoons at a time of the different foods.
A three-year-old child would be given three tablespoons at a time of the various foods.
So little food!
No, it is not too little if you keep in mind that toddlers have a very small stomach capacity and that
they cannot handle more food at a meal. This is also the reason why you need to give toddlers a
number of small meals every day and not expect them to eat large quantities at three main meals like
adults.
Many of the eating problems experienced during the first three years of life are due to the unrealistic
expectations of caring adults who cannot grasp the fact that their tiny child just cannot eat large
amounts of food and cannot thrive on only three meals a day. So do try and keep this fact in mind
when planning and preparing food for toddlers. Both the child and the parents will experience less
stress and meals will be pleasant, happy times if you offer the child portions that are suitable for the
child’s age and let the child eat six or more small meals a day.
Portion sizes and foods for toddlers aged two to three years
Food
Portions size
Number of serving
per day
Milk & dairy products
½ cup of milk or yoghurt or 15g cheese
4-5
Meat, fish, poultry,
eggs, peanut butter or
cooked legumes
30-60g meat, fish or poultry, 1 egg, 2 tablespoons
peanut butter or 4 tablespoons cooked legumes like 2
baked beans
Fruit & vegetables
4-5
Vegetables, cooked
2-3 tablespoons
Vegetables, raw
A few pieces - only if child can chew well
Fruit, raw
½-1 small fruit
Fruit, canned
2-4 tablespoons
Fruit juice
90-120ml (less than ½ cup)
Bread and cereals
3
Wholewheat or vitamin &
mineral fortified bread
½-1 slice
Cooked porridge
1/4-½ cup
Dry breakfast cereal
½-1 cup
Typical menu for toddlers aged two to three years
Breakfast:
40 ml fruit juice
1/4 cup oats porridge with 1 T honey
½ cup full cream milk
Mid-morning snack:
½ cup yoghurt
½ mashed, ripe banana
Lunch:
1 boiled egg
½ - 1 slice wholewheat bread with 1 t polyunsaturated margarine
½ grated apple
½ cup full cream milk
Mid-afternoon snack:
15 g sweetmilk or Gouda cheese
½ slice wholewheat bread with 1 t polyunsaturated margarine
40 ml fruit juice
Supper:
30 g cooked, mince meat
Mashed potato 2 T
Cooked butternut 1 T
1/4 cup custard
Bed-time snack:
1/4 cup full cream milk with Ovaltine
Breakfast
Day 1
Day 2
Day 3
Day 4
Apricot juice 40 ml
Orange juice 40 ml
Banana ½ mashed
Apple
Oats porridge 1/4 cup
Cornflakes, ½ cup
Egg 1 poached
Cream
Honey 1 T
Brown sugar 1 T
Toast ½-1 slice
Honey
Milk ½ cup
Millk ½ cup
Margarine 1 t
Yoghu
Milk ½ cup
Midmorningsnack
Lunch
Yoghurt ½ cup
Yoghurt ½ cup
Cheese 15g
Milk ½
Banana ½ mashed, ripe
Oats cookie 1
Apple juice 40 ml
Dried
Egg, 1 boiled
Peanut butter 2 T
Baked beans 3 T
Fish fi
Bread ½-1 slice
Bread ½-1 slice
Bread ½-1 slice
Mashe
Margarine 1 t
Margarine 1 t
Margarine 1 t
Canne
Apple ½ grated
Canned peach 1
Carrot sticks
Custar
Milk ½ cup
Milk ½ cup
Yoghurt 1/4 cup
Milk 1
Cheese
15gsweetmilk/Gouda
MidBread ½ slice
afternoonsnack
Margarine 1 t
Pear juice 40 ml
Supper
Cottage cheese 15g
Provitas 1-2
Peanu
Bread ½ slice
Margarine 1 t
Cracke
Margarine 1 t
Honey 1 T
Cranb
Apricot juice 40ml
Canned apricot 2
Meat 30g cooked mince
Fish cake, 30g
Potato, mashed 2 T
Pumpkin, 2 T
Butternut, cooked 1 T
Tomato, 2 slices
Custard 1/4 cup
Bedtimesnack
Yoghurt ½ cup
Meat 30g cooked
Egg, s
Carrots, cooked 2 T
Bread
Naartjie ½-1
Marga
Jelly
Banan
Milk ½ cup
Custar
Milk pudding 1/4 cup
Milk 1/4 cup withOvaltine Milk 1/4 cup with honey Milk 1/4 cup withHorlicks Milk 1
Notes:
The abovementioned menus are examples and can of course be varied according to season. Young
children do not need as much variety as older children, so that the menus for four days can be
repeated.
Bread - use wholewheat, brown or vitamin and mineral fortified bread.
Margarine - use polyunsaturated, soft or tub margarine.
Milk - use full cream milk (in contrast to adults, toddlers still need the energy supplied by the fat
content of full cream milk).
Fruit - use canned, cooked or pureed fruit for younger children.
Vegetables - use cooked or pureed vegetables with bland flavours for younger children, e.g. potato,
sweet potato, pumpkin, butternut, squash, carrots.
NASOGASTRIC TUBE FEEDINGS
Giving nasogastric tube feedings
Equipment:
Liquid food at room temperature and water in pour container
Feeding tube
Adhesive 1-cm or ½-inch tape
Water
Syringe
Stethoscope
Positioning for procedure:
On parent’s lap on infant’s right side,
or reclining him in an infant seat.
Measuring the tube for the exact distance (see fig.1):
Hold the tip of the tube on the child’s stomach (midway between the belly button and the highest
point of the lower rib cage).
Extend the tube up to the child’s ear lobe then out to his nose.
Mark the spot at the nose with the piece of tape.
Fig.1. Measuring the tube for the exact distance.
Inserting the tube
Dip the tip of the tube in clear water to moisten
Insert the tip of the tube into one nostril guiding it toward the back of the child’s throat
Ask the child to swallow or give him some water to help the tube pass
Quickly insert the tube to the tape mark on the tube.
If the child begins coughing or has any other problems, remove the tube at once.
Tape the tube to the child’s upper lip and cheek.
Check the placement of the tube
Place 5 cm³ of air in the syringe, connect the syringe to the tube
Place the stethoscope over the child’s stomach area.
Inject the air into the tube while listening for the sound of gurgling through the stethoscope.
With the syringe connected to the tube, gently pull back the plunger. If contents appear in the
tube, it is the correct place.
If not, place the child on the left side or advance the tube a short distance. Pull back on plunder
again to check for stomach contents.
Return the stomach contents.
Disconnect the syringe from the tube and remove the plunger from the syringe.
Reconnect the syringe to the tube.
Fig.2. The proper position of the syringe during nasogastric tube feeding.
Fill the syringe with the right amount of food.
If necessary push gently with the plunger to start the flow of food. Then remove the plunger and
allow the food to flow by gravity.
The bottom of the syringe should never be held higher than the child’s chin (See fig.2).
Continue adding food until the right amount has been fed. Do not allow the syringe to become
empty.
When the food is at the bottom of the syringe, add 1 teaspoon (5 ml) of water to rinse the tube.
Place the clamp on the tube if it will be left in place between feedings.
Hold, cuddle and burp the child.
Write down the time and amount of the child’s feeding.
To remove the tube:
Loosen the tape that is holding the tube.
Fold the tube and pinch it tightly together.
Pull the tube out quickly.
Hold, cuddle, and burp the child.
Care of the nasogastric tube and syringe
Wash with soap and water, and rinse the inside well with clear water.
Dry and store in a clean, dry container (e.g., plastic bag, margarine container).
If the tube remains in place between feedings, always check to make sure the tube is in the right
place before adding formula.
GASTROSTOMY FEEDING
Gastrostomy tubes are used to decompress the stomach or to offer feedings if the child is unable
to take nourishment orally. The tube is inserted surgically into the stomach through the
abdominal wall and is held in place by sutures or tape.
Equipment
20- to 50-cc syringe
Sterile water
Warmed feeding or formula
Procedure for Gastrostomy Feeding
Tubing is attached to a 20- to 50-cc syringe for feedings. Hold the child if possible; otherwise,
elevate his head and chest slightly (Figure 3-26). Elevate the syringe 10 to 12 centimeters (4 to 4
3/4 inches) and allow feeding to flow in by gravity. Never force the feeding. His condition
permitting, the infant may be given a pacifier to suck during the feeding to help fulfill his
sucking need, to relax him, and to help him equate the sucking reflex with the satisfaction of
hunger.
After feedings, do not clamp tubing unless physician has so ordered. Tubing may be elevated
after the feeding (Figure 3-27) and covered with a gauze square (A). This serves as a safety valve
and prevents gastric reflux and abdominal distention. It may be lowered and left open to provide
constant decompression (B); or it may be clamped in preparation for home care or removal (C).
If the tube is not be clamped, instill enough water to clean the tubing (10 to 30 milliliters,
depending on length of tubing), then clamp befor all of water leaves syringe. It the tube is to be
left open, it is not necessary to add water.
Record procedure accurately, including type and amount of feeding, amount of residual aspirate,
how child tolerated feeding, any abdominal distention, and activity after feeding.
TOTAL PARENTERAL NUTRITION
Total parenteral nutrition (TPN), or hyperalimentation, is a means of providing complete
nutrition by the intravenous route and is used when oral or gavage feedings are insufficient or
impossible. The TPN fluid contains water, protein, glucose, calories, vitamins, minerals, and
electrolytes. It is administered at a constant rate via an indwelling catheter and an infusion pump.
TPN may be used for several months.
The TPN fluid is prepared in the pharmacy under sterile conditions. It may be stored in the refrigerator for five days and hung at room temperature for no more than 24 hours. The fluid is
hypertonic and rich in nutrients; therefore, it is an excellent culture medium for bacteria. Every
precaution must be taken to avoid infection in the child because of the constant hazard of sepsis.
A millipore filter is used between the infusion tubing and the Silastic catheter to filter particulate
matter and/or microorganisms. Medications block the filter and are added via a Tconector between the filter and the Silastic catheter. (Controversy exists over the administration
of medications via the TPN tubing because of the danger of introducing infection or an air
embolus. If your institution adheres to the policy of not administering medications through the
TPN tubing, administer medications via a separate IV line.)
The flow rate is calculated by the physician for maximum glucose tolerance and should not
exceed 10 percent of the ordered rate per hour. Do not attempt to "catch up" TPN fluids because
the high osmolalityof the concentrated dextrose will cause hyperglycemia and an
osmotic diuresis leading to dehydration, seizures, and coma. Sudden reduction or cessation of the
flow rate will cause hypoglycemia. Monitor flow rate every hour to avoid these complications.
References
1. American Academy of Pediatrics Committee on Nutrition. Pediatric Nutrition Handbook. 3rd
edition. Elk Grove, Ill: American Academy of Pediatrics; 1993.
2. American Academy of Pediatrics Committee on Nutrition. Fluoride supplementation for
children: interim policy recommendations. Pediatrics. 1995; 95:77.
3. American Academy of Pediatrics Committee on Nutrition. Iron-fortified infant
formulas. Pediatrics. 1989; 84:1114.
4. American Academy of Pediatrics Committee on Nutrition. The use of whole cow’s milk in
infancy. Pediatrics. 1992;89:1105-1109.
5. American Academy of Pediatrics Committee on Nutrition. On the feeding of supplemental
foods to infants. Pediatrics. 1980;65:1178.
6. American Dietetic Association. Nutrition Management of the Infant. Manual of Clinical
Dietetics. 1997.
7. Cunningham AS, Jelliffe DB, Jelliffe EFP. Breastfeeding and health in the 1980’s; a global
epidemiologic review. J Pediatr. 1991;118:659-666.
8. Institute of Medicine. Nutrition During Lactation. Washington DC: National Academy of
Sciences; 1991.
9. Kaufman K, Hall L. Influences of the social network on choice and duration of breastfeeding in
mothers of preterm infants. Res Nurs Health 12: 149-59, 1989.
10. Kubit, JG. Lactation Issues in Groh-Wargo, Thompson, Cox (eds.) Nutritional Management
of High Risk Newborns. Chicago. Precept Press. pp.194-205, 1994.
11. Hopkinson JM, Garza C. Management of breastfeeding. In Tsang RC, Nichols BL (eds).
Nutrition During Infancy. St. Louis: CV Mosby, 1988: 298-313.
12. Wicker Stoker T. Common Nutrition Problems in Pediatrics in Hendricks and Walker (eds.)
2nd edition Manual of Pediatric Nutrition, Toronto, B.C. Decker, 1990; 145.
13. Lawrence RA. Breastfeeding - A Guide for the Medical Profession. 3rd edition. St.
Louis, Mo: CV Mosby Co; 1989.
14. Groh-Wargo and Antonelli K. Normal Nutrition During Infancy in Queen PM and Lang CE
(eds.) The Handbook of Pediatric Nutrition, Gaithersburg, Aspen Publishers; pp. 107-144. 1993.
15. Lucas A. Enteral Nutrition in Tsang, RC, Lucas A, Uauy R and Zlotkin S (eds.) Nutritional
Needs of the Preterm Infant: Scientific Basis and Practical Guidelines, Pawling, NY, Caduceus
Medical Publishers for Williams & Wilkins, pp. 209-221, 1993.
16. Jakobsson I, Lindberg T. Cow's milk proteins cause infantile colic in breast fed infants: a
double-blind crossover study. Pediatrics 1983;71:268.
17. Berlin CM, Denson HM, Daniel CH, Ward RM. Deposition of dietary caffeine in milk, saliva,
and plasma of lactating women. Pediatrics. 1984;73:59.
18. Luck W, Nau H. Nicotine and cotinine concentrations in serum and urine of infants exposed
via passive smoking or milk from smoking mothers. J Pediatr. 1985;107;2:275.
19. Binkieewicz A, Robinson JM, Senior B. Pseudo-Cushing syndrome caused by alcohol in
breast milk. J Pediatr. 1978;93:965.
20. Ewek AK, Durbin GM, Morgan ME and Booth IW. Gastric Emptying in Preterm Infants.
Archives of Disease in Childhood: Fetal and Neonatal Edition. 71(1):F24-7, July 1994.
21. Ewer AK. Gastric emptying of preterm infants: the effect
of breastmilk fortifier. Acta Paediatrica. 85(9):1112-5, September 1996.
22. Anderson GH, Atkinson SA, Bryan MH. Energy and macronutrient content of human milk
during early lactation from mothers giving birth prematurely and at term. Am J Clin Nutr. 34:258,
1981.
23. Lemons JA, Moye L, Hall D, et al. Differences in the composition of preterm and term human
milk during early lactation. Pediatr Res 16:113, 1982.
24. Fomon SJ, Ziegler EE, Vasquez AD. Human milk and the small premature infant. Am
J Dis Child. 1977:131:462.
25. Sapsford, AL. Appendix O: Composition of Human Milk, Selected Infant Formulas, and
Modular Supplements in Groh-Wargo S, Thompson, M and Hovasi Cox J. Nutritional Care for
High-Risk Newborns, Chicago, Precept Press, Inc., pp. 422, 1993.
26. Mead Johnson Product Handbook, 1996.
27. Eiger MS, Wendkos S. The Complete Book of Breastfeeding. New York, Workman
Publishing, pp. 224-5, 1987.
28. Hansen JW, Cook DA, Cordano A, Miguel SG. Human Milk Substitutes in Tsang RC and
Nichols BL (eds.) Nutrition During Infancy St. Louis, CV Mosby Company 378-398, 1988.
References
1. Waller, Bruce N. 2005. Consider Ethics: Theory, Readings, and Contemporary Issues. New
York: Pearson Longman: 23.
2. Beauchamp, Tom L. 1991. Philosophical Ethics: An Introduction to Moral Philosophy, 2nd
Ed. New York: McGraw Hill: 171.
3. Waller, Bruce N. 2005. Consider Ethics: Theory, Readings, and Contemporary Issues. New
York: Pearson Longman: 23.
4. Orend, Brian. 2000. War and International Justice: A Kantian Perspective. West Waterloo,
Ontario:Wilfrid Laurier University Press: 19.
5. Kelly, Eugene. 2006. The Basics of Western Philosophy. Greenwood Press: 160.
6.
Kamm, F. M. 1996. Morality, Mortality Vol. II: Rights, Duties, and Status. New York:
Oxford University Press.
7. Kamm, F. M. 2007. 'Chapter 5: Toward the Essence of Nonconsequentialist Constraints on
Harming.'. In Intricate Ethics: Rights, Responsibilities, and Permissible
Harm. Oxford: Oxford UniversityPress.
8.
Kamm, F. M. 1996. Morality, Mortality Vol. II: Rights, Duties, and Status. New York:
Oxford University Press.
9. Kamm, F. M. 2007. Intricate Ethics: Rights, Responsibilities, and Permissible Harm. New
York: Oxford University Press.
10. Waller, Bruce N. 2005. Consider Ethics: Theory, Readings, and Contemporary Issues. New
York: Pearson Longman.
11. Booth, J (1977). "A short history of blood pressure measurement". Proceedings
of the Royal Society of Medicine 70 (11): 793–9.
12. Watson, S.; Wenzel, R. R.; di Matteo, C.; Meier, B.; and Lüscher, T. F. (1998). "Accuracy of
a new wrist cuff oscillometric blood pressure device". American Journal of Hypertension 11:
1469-1474 (1998).
13. Usichenko, TI; Pavlovic D, Foellner S & Wendt M. (2004). "Reducing venipuncture pain by
a cough trick: a randomized crossover volunteer study". Anesthesia and Analgesia 99 (3):
952–3.
14. Anesthesia and Analgesia 2004;98:343-5
15. Harrison, D; Stevens B, Bueno M, Yamada J, Adams-Webber T, Beyene J, Ohlsson A.
(2010). "Efficacy of sweet solutions for analgesia in infants between 1 and 12 months of age:
a systematic review.". Archives of Disease in Childhood 95 (6): 406–13.
16. How to take your child's temperature. American Academy of Pediatrics.
http://patiented.aap.org/content.aspx?aid=6368. Accessed Jan. 15, 2010.
17. Shelov SP, et al. Caring For Your Baby And Young Child: Birth To Age 5. New York, N.Y.:
Bantam; 2009:747.
18. Bobb B, et al. Fever and sweats. In: Walsh D, et al. Palliative medicine. Philadelphia, Pa.:
Saunders Elsevier; 2009. http://www.mdconsult.com/das/book/body/1715874494/0/2038/167.html?tocnode=57251154&fromURL=167.html. Accessed Nov. 16, 2009.
19. Powell KR. Fever. In: Kliegman RM, et al. Nelson Textbook of Pediatrics. 18th
ed. Philadelphia, Pa.: Saunders Elsevier; 2007.
http://www.mdconsult.com/das/book/body/1715874494/0/1608/510.html?tocnode=54478711&fromURL=510.html#4-u1.0-B978-1-4160-24507.50176-6_3974. Accessed Nov. 16, 2009.
20. How to take a child's temperature. American Academy of Pediatrics.
http://www.healthychildren.org/English/health-issues/conditions/fever/Pages/How-to-Take-aChilds-Temperature.aspx. Accessed Feb. 12, 2010.
21. Holzhauer JK, et al. Evaluation of temporal artery thermometry in children 3-36 months
old. Journal for Specialists in Pediatric Nursing. 2009;14:239.
22. Medications used to treat a fever. American Academy of Pediatrics.
http://www.healthychildren.org/English/health-issues/conditions/fever/pages/MedicationsUsed-to-Treat-Fever.aspx. Accessed Feb. 12, 2010.
23. Braun CA. Accuracy of pacifier thermometers in young children. Pediatric Nursing.
2006;32:413.
24. Hoecker JL (expert opinion). Mayo Clinic, Rochester, Minn. Feb. 15, 2010.